This study examines the relationship between remnant cholesterol, glucose metrics, and chronic complications of type 1 diabetes in users of glucose monitoring systems.
Material and methodsClinical variables and glucose metrics were collected from individuals using glucose sensors. Statistical models were employed to investigate the association of remnant cholesterol with glucose metrics, diabetic retinopathy, and diabetic nephropathy.
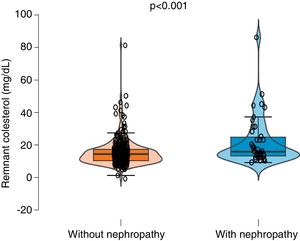
ResultsA total of 383 individuals, aged 48.3 ± 16.2 years, with 54.1% women, and a remnant cholesterol level of 16 ± 10 mg/dL, were included. The results demonstrated that remnant cholesterol was associated with less time within the target range (p = 0.015) and more time above the target range (p = 0.003). Diabetic nephropathy was the only complication associated with remnant cholesterol levels exceeding 30 mg/dL, OR 8.93, 95% CI (2.99–26.62), p < 0.001.
ConclusionRemnant cholesterol is independently associated with hyperglycemia and diabetic nephropathy in individuals with type 1 diabetes.
Este trabajo investiga la relación entre el colesterol remanente, las métricas de glucosa y las complicaciones crónicas de la diabetes tipo 1 en individuos con sistemas flash de glucosa.
Material y métodosSe recopilaron variables clínicas y métricas de glucosa de personas usuarias de sensores de glucosa. Se llevaron a cabo modelos estadísticos para estudiar la asociación del colesterol remanente con las métricas de glucosa, así como con la retinopatía y nefropatía diabética.
ResultadosSe incluyeron 383 personas con una edad de 48,3 ± 16,2 años, siendo un 54,1% mujeres, con un colesterol remanente de 16 ± 10 mg/dL. Los resultados mostraron que el colesterol remanente se asocia a un menor tiempo en rango (p = 0,015) y a un mayor tiempo por encima del rango (p = 0,003). La nefropatía diabética fue la única complicación que se asoció con un colesterol remanente mayor a 30 mg/dL, OR 8,93 IC 95% (2,99–26,62) p < 0,001.
ConclusiónEl colesterol remanente se asocia de forma independiente con la hiperglucemia y la nefropatía diabética en personas con diabetes tipo 1.
Remnant cholesterol (C-REM) is the cholesterol content present in triglyceride-rich lipoproteins, including both very low-density lipoproteins and intermediate-density lipoproteins, in the fasting state. Additionally, it encompasses remnants of chylomicrons in non-fasting situations.1 The indirect estimation of remnant cholesterol is calculated by subtracting LDL cholesterol and HDL cholesterol from total cholesterol.2 When C-REM particles reach the intima layer of arteries, they are captured by macrophages, leading to the formation of foam cells and promoting atherosclerosis.1 Also, the degradation of triglycerides in these particles results in the release of free fatty acids and monoacylglycerols, triggering an inflammatory cascade.3 Individuals with remnant cholesterol concentrations exceeding 30 mg/dL have been observed to potentially have a higher prevalence of arteriosclerotic disease.4
The impact of C-REM on glycemic control and complications of type 1 diabetes (DM1) has been poorly studied until now.5 In this regard, the widespread implementation of continuous glucose monitoring systems, in addition to improving glycemic control, can provide new insights into the determining factors of disease control, given the large number of people using these systems and the vast amount of data they generate.6
The objective of this study was to examine the relationship between C-REM and glucose metrics, as well as chronic complications in individuals with DM1 using flash glucose monitoring systems (FGM).
Materials and methodsA cross-sectional study in the context of routine clinical practice was conducted in February 2023 at a tertiary hospital in Madrid, Spain. Participants included patients diagnosed with DM1 under regular follow-up at the center and regular users of the FreeStyle Libre® flash glucose monitoring system by Abbott. Individuals with other types of diabetes, those with a sensor usage time <70%, as per recommendations,6 and those with missing clinical variables were excluded. Clinical variables such as age, sex, duration of diabetes, insulin dose, glycated hemoglobin (HbA1c), fasting cholesterol fractions (total, HDL, and LDL calculated using the Friedewald equation), statin treatment, and the presence of diabetic nephropathy and retinopathy were collected. Glucose metrics, such as the percentage of time in the range 70–180 mg/dL (TIR), percentage of time above range >180 mg/dL (TAR), and percentage of time below range <70 mg/dL (TBR), were downloaded from the Libreview information cloud for 14 days. C-REM was calculated as the difference between total cholesterol and the sum of HDL and LDL. Diabetic nephropathy and retinopathy were classified binary based on international standards.7,8 Excess C-REM was considered when it exceeded 30 mg/dL.4
Statistical analysisThe normality of variables was assessed using the Kolmogorov–Smirnov test. To evaluate differences between non-normal variables, the Wilcoxon test was employed, and for normal variables, the Student’s t-test was used. The relationship between variables was explored through correlation analysis. Multivariable linear regression models were conducted to study the impact of C-REM on clinical variables, glycemic control, and complications independently. Logistic regression models were also employed to investigate the impact of various variables on excess C-REM.
Statistical analysis was performed using STATA 17.0 BE-Basic edition (Lakeway Drive, College Station, Texas, USA) and R, version 4.0.3. A p-value <0.05 was considered statistically significant.
Ethical considerationsAll patients included in the study were informed of its objectives and agreed to the use of their clinical data for research purposes. The Research Ethics Committee of La Princesa Hospital in Madrid approved this study (study number: 2022-4997-17/22).
ResultsSample characteristicsAfter applying the inclusion and exclusion criteria, 383 subjects with type 1 diabetes (DM1) who were regular users of the FreeStyle Libre 2 flash glucose monitoring system were included. The mean age of the sample was 48.3 ± 16.2 years, with 54.1% of participants being women. All individuals were undergoing multiple insulin dose therapy. The mean total cholesterol of the sample was 173 ± 37 mg/dL, and C-REM was 16 ± 10 mg/dL. A total of 106 individuals (27.6%) had some degree of diabetic retinopathy, and 52 (13.5%) had diabetic nephropathy. One hundred seventy individuals (44%) were on statin therapy, including 6 (3.5%) with low intensity, 107 (62.9%) with moderate dose, and 57 (33.5%) with high dose. Glucose metrics and other characteristics of the sample are presented in Table 1.
Sample characteristics.
| Variables | Observation n = 383 |
|---|---|
| Age (years) | 48.3 ± 16.2 |
| Female gender | 207 (54.1%) |
| Duration of diabetes (years) | 21.6 ± 13.9 |
| HbA1c (%) | 7.18 ± 1.0 |
| Total cholesterol (mg/dL) | 173 ± 37 |
| HDL cholesterol (mg/dL) | 58 ± 16 |
| LDL cholesterol (mg/dL) | 99 ± 31 |
| Remnant cholesterol (mg/dL) | 16 ± 10 |
| Remnant cholesterol >30 mg/dL | 28 (7.4%) |
| % Time in range (70–180 mg/dL) | 65.2 ± 17.6 |
| % Time above range (>180 mg/dL) | 30.1 ± 18.3 |
| % Time below range (<70 mg/dL) | 4.7 ± 5.34 |
| Sensor readings/daily | 11.7 ± 7.6 |
| Sensor wear time (years) | 1.7 ± 0.8 |
| Insulin dose/kg/day | 0.57 ± 0.22 |
| Diabetic retinopathy | 106 (27.6%) |
| Diabetic nephropathy | 52 (13.5%) |
HbA1c: glycated hemoglobin.
The results showed a negative association between TIR and C-REM levels (Spearman’s Rho = −0.1246; p = 0.019) and a positive association with TAR (Rho = 0.147; p = 0.006). A negative association was also observed between TBR and C-REM (Rho = −0.14; p = 0.005).
Multivariate linear regression models for the TIR variable demonstrated that C-REM is an independent negative factor (β −0.26, 95% CI −0.46 to −0.05; p = 0.015) in a model adjusted for age, sex, duration of diabetes, smoking, daily sensor readings, insulin dose, total cholesterol, and LDL cholesterol. Age, female sex, and the number of readings were positively and significantly associated (p < 0.05) with higher TIR, while active smoking and insulin doses were negatively associated with TIR (p < 0.05). Total cholesterol, LDL, and duration of diabetes did not show significant implications for TIR (p > 0.05). The adjusted R2 of the model was 0.216, p < 0.001.
The linear regression model for the TAR > 180 mg/dL variable also showed that C-REM is associated with a longer time above range (β 0.33, 95% CI 0.12 to −0.56; p = 0.003) in a model adjusted for the same covariates. Age, female sex, and the number of readings were associated with a shorter TAR (p < 0.05), while active smoking and insulin doses were associated with a longer TAR (p < 0.05). Total cholesterol, LDL, and duration of diabetes did not show significant implications for TAR (p > 0.05). The adjusted R2 of the model was 0.166, p < 0.001.
Relationship of remnant cholesterol with diabetic retinopathy and nephropathyThe study of C-REM values in individuals with diabetic nephropathy showed significantly higher levels in those with diabetic nephropathy (21.7 ± 14.9 mg/dL) compared to those without it (15.0 ± 9.2 mg/dL, p < 0.001) (Fig. 1). No statistically significant differences were observed in C-REM values in individuals with diabetic retinopathy compared to those without it (p = 0.693).
A stepwise multivariable logistic regression model was performed for the C-REM >30 mg/dL variable, including all clinical variables, glucose metrics, and the presence of diabetic nephropathy and retinopathy. The results showed that the only factor significantly associated with excess C-REM was diabetic nephropathy, with an Odds Ratio of 8.93, 95% CI (2.99–26.62), p < 0.001.
DiscussionScientific evidence supporting the use of C-REM as an important parameter in assessing cardiovascular risk and complications of diabetes mellitus has grown in recent years.5 This study aimed to examine the association between C-REM and glucose metrics in the chronic control of DM1. Our data show that C-REM levels are associated with lower TIR, higher TAR, and the coexistence of diabetic nephropathy.
Studies evaluating C-REM levels in people with DM1 are scarce, and to our knowledge, they have not been studied in relation to metrics from flash glucose monitoring. In our work, C-REM is associated with lower TIR and higher TAR, implying poorer glycemic control that could explain the relationship with the onset of chronic complications of DM1 that have already been documented.5 Our data also show an association between higher TBR and lower C-REM levels, but this data should be interpreted with caution due to the low TBR rate in the sample. On the other hand, in line with previous studies,5 we observed higher C-REM levels among people with diabetic nephropathy compared to those who did not have it. Additionally, regression models have shown that the presence of diabetic nephropathy is the only factor significantly associated with fasting C-REM levels >30 mg/dL, considered the pathological threshold.9 However, no differences or associations were observed between C-REM and diabetic retinopathy.
This study has several limitations. Firstly, it is a retrospective observational study, so the ability to establish causality is limited to hypothesis formulation. Secondly, the number of patients treated with statins (44%) prevents regression models with a sufficient sample to assess their impact on C-REM. However, in the statistical analysis, no differences were observed between different treatment intensities, making the role of this implication uncertain. Lastly, C-REM was measured indirectly in this study, although it is a validated measurement to identify cardiovascular risk.2
ConclusionsC-REM is a variable of growing interest in the study of metabolic and vascular pathology. Our study shows that C-REM is independently associated with worse glucose metrics and diabetic nephropathy in DM1 patients using flash glucose systems. Further research will be necessary to investigate the effects of C-REM in DM1 in future studies.
Conflicts of interestThe authors declare that they have no conflicts of interest.
FundingThis research work has received no research grants or funds from public, private, or commercial agencies or agencies of any other type.
Ethical considerationsThis study was carried out in accordance with the principles of the Declaration of Helsinki. This study was approved by the Ethics Committee of our center (The Research Ethics Committee of the Hospital de La Princesa, Madrid, approved this study (study number: 2022-4997-17/22). Informed consent was obtained from all individual participants included in the study. In view of the retrospective nature of the study, all procedures performed were part of routine care.