Real-world studies evaluating the impact of 2019 European Societies of Cardiology (ESC) and Atherosclerosis (EAS) guidelines on the use of lipid-lowering treatments (LLTs) are scarce. This manuscript shows baseline and 1-year follow-up data on LLT usage and low-density lipoprotein cholesterol (LDL-C) goal attainment in the Spanish subpopulation from SANTORINI study and put them in perspective with the European cohort without Spanish participants.
MethodsSANTORINI was a multinational, prospective, non-interventional study. The Spanish subpopulation involved up to 1018 patients at high and very high cardiovascular (CV) risk.
ResultsOf 956 patients in LDL-C dataset, mean LDL-C levels decreased from baseline (82.7 ± 40.6 mg/dL) to 1-year follow-up (72.3 ± 32.6 mg/dL), in patients at high and very high risk. The percentage of patients who achieved 2019 ESC/EAS LDL-C goals increased from 26.5% at baseline to 34.1% at 1-year follow-up, in patients at high (23.1% versus 27.3%) and very high risk (27.9% versus 37.0%). Attainment to LDL-C targets improved while initiating treatment with a LLT in patients not receiving it at baseline or following change to a combination therapy in those who were receiving it. During the follow-up, seven patients died due to CV causes, and 46 and 24 had at least one four- or three-component major adverse CV events, respectively.
ConclusionsFollow-up data from SANTORINI Spain show that LLT usage increased from baseline, including monotherapy and combination therapy. Despite recommendations, patients at highest CV risk continue not receiving the most adequate LLT for reducing LDL-C levels in routine clinical practice.
Los estudios en vida real que han evaluado el impacto de las guías de 2019 de la Sociedad Europea de Cardiología (ESC) y la Sociedad Europea de Aterosclerosis (EAS) sobre el uso de tratamientos hipolipemiantes (LLT) son escasos. Este manuscrito presenta los datos basales y tras un año de seguimiento del uso de LLT y la consecución de objetivos de colesterol de lipoproteínas de baja densidad (LDL-C) en la subpoblación española del estudio SANTORINI y los pone en perspectiva con la cohorte europea sin participantes españoles.
MétodosSANTORINI fue un estudio multinacional, prospectivo y observacional. La subpoblación española incluyó hasta 1018 pacientes con riesgo cardiovascular (CV) alto y muy alto.
ResultadosEn los 956 pacientes con datos de LDL-C, los niveles medios de LDL-C disminuyeron desde la visita basal (82,7 ± 40,6 mg/dL) hasta la de un año de seguimiento (72,3 ± 32,6 mg/dL) en pacientes con riesgo alto y muy alto. El porcentaje de pacientes que alcanzaron los objetivos de LDL-C, según las guías ESC/EAS de 2019, aumentó del 26,5% en la visita basal al 34,1% tras un año de seguimiento, tanto en pacientes de riesgo alto (23,1% versus 27,3%) como muy alto (27,9% versus 37,0%). La consecución de objetivos de LDL-C mejoró al iniciar tratamiento con un LLT, en pacientes que no lo recibían en la visita basal, o al cambiar a una terapia combinada, en aquellos que ya lo estaban recibiendo. Durante el seguimiento, siete pacientes fallecieron por causa CV y 46 y 24 experimentaron al menos uno de los eventos adversos CV mayores de cuatro y tres componentes, respectivamente.
ConclusionesLos datos de seguimiento de SANTORINI España muestran que el uso de LLT aumentó desde la visita basal, tanto la monoterapia como la terapia combinada. A pesar de las recomendaciones, los pacientes con mayor riesgo CV siguen sin recibir el tratamiento hipolipemiante más adecuado para reducir sus niveles de LDL-C en la práctica clínica habitual.
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity in Europe, resulting in 3.9 million deaths every year.1 Low-density lipoprotein cholesterol (LDL-C) plays a pivotal role in the development of atherosclerosis and plaque formation, resulting in impaired blood flow and an elevated risk of cardiovascular (CV) events.2 For this reason, reducing LDL-C levels has become a cornerstone for CVD prevention.3 In fact, a decline of one mmol/L in LDL-C has been associated with a relative risk reduction of up to 23% in major vascular and coronary events, as well as a 10% decrease in total mortality over a 5-year period.4,5 Consequently, the 2019 update of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) guidelines recommended more stringent LDL-C targets, i.e. below 70 mg/dL (<1.8 mmol/L) and 55 mg/dL (<1.4 mmol/L) for patients at high and very high CV risk, respectively, together with a minimum 50% reduction in LDL-C levels from baseline.5 To cope such aim, combination therapy (involving statins and non-statin lipid-lowering treatments, LLTs) is highly recommended for these patients.6,7 In statin-naïve patients, combination therapy with ezetimibe and statin has resulted in approximately 15% greater LDL-C reduction compared to statin monotherapy at same doses.5,8 Additionally, this combination has led to more significant LDL-C reductions compared to doubling the statin dose (13–20%) and switching from statin monotherapy to ezetimibe and statin combination therapy (11–15%). Over the past decade, real-world studies using less stringent LDL-C thresholds have consistently demonstrated that many patients, including those at high and very high risk, fail to reach the recommended LDL-C levels.9–13 These studies have also evidenced that LLTs are mainly statin-based monotherapy, and that combination therapy is used by a minority. To date, real-world studies evaluating the impact of 2019 ESC/EAS guidelines on the use of LLTs are scarce.14,15
The SANTORINI was a prospective, multinational, observational study aimed at evaluating the implementation of the 2019 update of the ESC/EAS guidelines in adult patients at high and very high CV risk from 14 European countries between 2020 and 2021.16 Baseline results of 9136 patients revealed that 20.9% of them were not receiving LLTs, 53.6% were treated with LLT monotherapy, and 25.6% were on combination therapy. Out of the 7,210 patients with complete baseline and follow-up LDL-C data, goal attainment increased from 21.2% at baseline to 30.9% at 1-year follow-up.16 LLTs were escalated in one third of patients. The use of monotherapy and combination therapy (n = 9136) also rose (from 53.6% to 57.1%, and from 25.6% to 37.9%, respectively).16
In the present manuscript we present the baseline and 1-year follow-up data on the LLT usage and LDL-C goal attainment in the Spanish subpopulation from SANTORINI (namely SANTORINI Spain) and show the results in perspective with respect to the European cohort without Spanish participants (namely SANTORINI Europe without Spain).
MethodsStudy design and patientsThe SANTORINI (NCT04271280) study was an observational, non-interventional study that enrolled adult patients who were at high or very high risk (according to the physicians who were attending them), were eligible for LLTs, and had a life expectancy greater than one year at the time of the study inclusion.17 No exclusion criteria were required. Patients were enrolled between March 2020 and February 2021, and then were followed-up for 12 ± 2 mo from baseline. Recruited patients could be either in primary or secondary prevention. The SANTORINI study was carried out in accordance with the Declaration of Helsinki. All patients signed a written informed consent to participate in the study.
Objectives and variablesThe primary objective of SANTORINI was to describe the LLTs currently employed in routine clinical practice in patients at high and very high risk, and to assess the proportion of those who meet the recommended 2019 ESC/EAS LDL-C targets.5 The CV risk for each patient was determined at the time of the enrollment by the physicians who attended them. Thresholds for LDL-C goals were <70 mg/dL (<1.8 mmol/L) for patients at high risk and <55 mg/dL (<1.4 mmol/L) for those at very high risk.5 The CV risk during the follow-up was determined as a secondary objective. It was measured by means of the CV death, four-component major adverse CV events (MACE), three-component MACE, and the event rate per 100 patient-years (PY). The four-component MACE was defined as when occurring any of the following events: CV death, non-fatal myocardial infarction, non-fatal stroke, or coronary revascularization (coronary artery bypass grafting surgery and/or percutaneous transluminal coronary angioplasty). The three-component MACE was defined as when occurring any of the following events: death from CV causes, non-fatal myocardial infarction, or non-fatal stroke. Event rate per 100 PY was calculated as the number of patients with the CV event (based on the time to the first event only) divided by the total exposure time for all patients at risk (years) multiplied by 100.
In the present manuscript we also fulfill the objectives using the data from SANTORINI Europe without Spain, i.e. SANTORINI Europe but excluding data from Spain, in order to put the Spanish results into perspective with Europe. Information on intensity of LLTs has been detailed elsewhere.18
Statistical analysisOnly descriptive analyses have been conducted in the present observational study. Continuous variables are shown as mean ± standard deviation (SD), whereas categorical ones as absolute and relative frequencies (%). Results are shown in the overall population and regarding the CV risk determined by the physicians. LDL-C levels are presented in mg/dL (to convert into mmol/L, values must be multiplied by 0.02586). Patient characteristics, LLT usage, and CV risk were evaluated in patients with any available follow-up data (i.e. full analysis set), whereas LDL-C levels and goal attainment in those with LDL-C data available at both baseline and 1-year follow-up (i.e. LDL-C dataset). Confidence intervals for LDL-C goal attainment and CV event rates were calculated using Clopper-Pearson methodology. All analyses were performed in SAS version 9.4, SAS Institute Inc., Cary, NC, USA.
ResultsBaseline patient’s characteristics in SANTORINI SpainOut of 1043 recruited patients in Spain, 1018 were included in the full analysis set and 956 in the LDL-C dataset. The patient flow diagram (with reasons for exclusion) is shown in the Supplementary Fig. 1. Overall, patients were predominantly male (72.9%), with a mean age of 63.3 ± 11.3 years, and a body mass index of 28.4 ± 4.7 Kg/m2 (Table 1). A high percentage of patients showed atherosclerotic cardiovascular disease (ASCVD, 67.4%), hypertension (62.9%), and diabetes (41.4%). Of patients, 14.8% had heterozygous familial hypercholesterolemia. According to the physicians, 295 patients (29.0%) were classified as high risk and 723 (71.0%) as very high risk.
Baseline characteristics in SANTORINI Spain for overall, LDL-C dataset, and risk classification as reported by physicians (full analysis set).
| Risk classification as reported by physicians (full analysis set)* | ||||
|---|---|---|---|---|
| Patient characteristics | Overall* (N = 1018) | LDL-C dataset** (N = 956) | High risk (N = 295) | Very high risk (N = 723) |
| Male, n (%) | 742 (72.9) | 689 (72.1) | 175 (59.3) | 567 (78.4) |
| Age, mean ± SD years | 63.3 ± 11.3 | 63.0 ± 11.3 | 59.6 ± 12.6 | 64.8 ± 10.4 |
| ASCVD, n (%) | 686 (67.4) | 634 (66.3) | 48 (16.3) | 638 (88.2) |
| BMI, mean ± SD Kg/m2 | 28.4 ± 4.7 | 28.4 ± 4.7 | 28.1 ± 4.8 | 28.5 ± 4.7 |
| Systolic blood pressure, mean ± SD mmHg | 132.6 ± 18.5 | 132.7 ± 18.4 | 134.2 ± 18.1 | 131.9 ± 18.6 |
| Diastolic blood pressure, mean ± SD mmHg | 76.8 ± 11.4 | 76.8 ± 11.3 | 79.0 ± 11.3 | 75.9 ± 11.3 |
| Hypertension, n (%) | 640 (62.9) | 592 (61.9) | 147 (49.8) | 493 (68.2) |
| Diabetes, n (%) | 421 (41.4) | 387 (40.5) | 105 (35.6) | 316 (43.7) |
| eGFR, mean ± SD mL/min/1.73 m2 | 80.6 ± 23.9 | 81.2 ± 23.6 | 85.6 ± 22.8 | 78.6 ± 24.1 |
| Heterozygous familial hypercholesterolemia, n (%) | 151 (14.8) | 147 (15.4) | 96 (32.5) | 55 (7.6) |
| Smoking history, n (%) | ||||
| Current | 164 (16.1) | 157 (16.4) | 57 (19.3) | 107 (14.8) |
| Former | 495 (48.6) | 461 (48.2) | 102 (34.6) | 393 (54.4) |
| Never | 359 (35.3) | 338 (35.4) | 136 (46.1) | 223 (30.8) |
| LDL-C#, mean ± SD | 82.4 ± 40.8 | 82.7 ± 40.6 | 102.0 ± 46.4 | 74.4 ± 35.2 |
ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index; SD, standard deviation; eGFR, estimated glomerular filtration rate; LDL-C, low-density lipoprotein cholesterol.
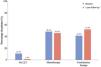
Overall, 48.1% and 41.2% of patients were receiving LLT monotherapy and combination therapy at baseline, respectively (Fig. 1 and Supplementary Table 1). The use of LLT monotherapy in patients at high and very high risk was 47.8% and 48.3%, whereas the use of combination therapy was 40.3% and 41.5%. At 1-year follow-up, the percentage of overall LLT monotherapy use slightly decreased (45.5%) whereas the combination therapy use raised (51.8%). At this time, the use of LLT monotherapy was 48.5% and 44.2% in patients at high and very high risk, and the use of combination therapy was 49.5% and 52.7% in those at high and very high risk. The increase in the use of combination therapy was mainly observed in patients with ASCVD (from 43.6% to 56.4%) and in a lesser degree in those without ASCVD (from 36.1% to 42.2%; Supplementary Table 2). Overall, 10.7% of patients were not receiving LLTs at baseline; percentage that dropped to 1.3% at 1-year follow-up. During the period of time, therapy was unchanged in most patients (73.1%; Supplementary Table 3). It was escalated in 22.4% of patients and de-escalated in 3.1%.
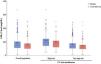
LDL-C levels and goal attainment in SANTORINI SpainOverall, mean LDL-C levels decreased from baseline (82.7 ± 40.6 mg/dL) to 1-year follow-up (72.3 ± 32.6 mg/dL), in both patients at high (from 101.4 ± 46.3 mg/dL to 88.7 ± 37.1 mg/dL) and very high risk (from 74.7 ± 35.0 mg/dL to 65.4 ± 27.7 mg/dL; Fig. 2). The percentage of patients who achieved the 2019 ESC/EAS LDL-C goals increased from 26.5% at baseline to 34.1% at 1-year follow-up, in both patients at high (23.1% versus 27.3%) and very high risk (27.9% versus 37.0%; Fig. 3). This raise was especially notable in the population of patients who were not receiving LLT at baseline, in whom goal attainment increased from 8.6% at baseline to 32.4% at 1-year follow-up (Supplementary Fig. 2).
During the follow-up, seven patients died due to CV causes, all of them at very high risk (Supplementary Table 4). Of patients, 46 and 24 had at least one four- or three-component MACE, respectively. Therefore, event rates corresponded to 0.7 (95% confidence interval, 95% CI: 0.2–1.2) CV deaths, 4.6 (95% CI: 3.3–5.9) four-component MACE, and 2.4 (95% CI: 1.4–3.3) three-component MACE per 100 PY of follow-up.
Perspective with SANTORINI Europe without SpainWhen showing data in relation with SANTORINI Europe without Spain, the use of combination therapy after 1-year follow-up was greater in Spain than in Europe (51.8% versus 36.2%; Fig. 4). In patients at high risk, the use of LLT monotherapy in Spain was 48.5% compared to 68.3% in Europe, and the use of combination therapy in Spain was 49.5% versus 24.1% in Europe (Supplementary Table 5). In patients at very high risk, the use of LLT monotherapy in Spain was 44.2% compared to 54.6% in Europe, and the use of combination therapy in Spain was 52.7% versus 41.1% in Europe.
In SANTORINI Europe without Spain, mean LDL-C levels decreased from 95.2 ± 47.8 mg/dL at baseline to 77.4 ± 37.1 mg/dL after 1-year follow-up (Supplementary Table 6). The percentage of patients who achieved their LDL-C targets increased from 20.4% to 30.4%. In SANTORINI Europe without Spain, during the follow-up, 81 patients died due to CV causes, and 451 and 189 had at least one four-or three-component MACE, respectively (Supplementary Table 7). Thus, event rates corresponded to 1.0 (95% CI: 0.8–1.2) CV deaths, 5.7 (95% CI: 5.2–6.3) four-component MACE, and 2.4 (95% CI: 2.0–2.7) three-component MACE per 100 PY of follow-up.
DiscussionThe present results from SANTORINI Spain reveal an increase in LLT use and in the percentage of patients achieving the recommended 2019 ESC/EAS LDL-C targets after 1-year of follow-up. Real-world studies conducted before the publication of the 2019 ESC/EAS guidelines already revealed the suboptimal LDL-C goal attainment in patents at high and very high risk.9–13 At the same time, the studies highlighted that these patients were not receiving the most adequate LLT for reducing their LDL-C levels. In DA VINCI study, carried out between 2017 and 2018, 63% of patients at high risk and 39% at very high risk achieved the 2016 ESC/EAS risk-based goals.12 In addition, the study showed that 84% of LLTs were statin-based monotherapy, whereas 10% was represented by combination therapy. After the 2019 update of the ESC/EAS guidelines only few studies have evaluated the implementation of the more stringent LDL-C thresholds and the usage of LLTs in routine clinical practice.14,15 In Europe, SANTORINI has reported a change in LDL-C attainment from 21.2% at baseline to 30.9% after 1-year of follow-up in the 7210 patients with complete LDL-C data.16 The usage of LLT monotherapy increased from 53.6% to 57.1%, and combination therapy from 25.6% to 37.9%. In fact, a better LDL-C control was reported in patients who were receiving combination therapy. Numerous studies have evidenced the use of combination therapy, both oral (statins, ezetimibe, and bempedoic acid) and subcutaneous (adding PCSK9 inhibitors) for substantially reducing LDL-C, specifically in patients at highest CV risk.6,19–22 In the multicenter, randomized, double-blind, placebo-controlled FOURIER20 and ODYSSEY21 trials, the addition of evolocumab or alirocumab to high-intensity statin therapy decreased the risk for CV events by 15% over approximately two years. In the Treat Stroke to Target study, 2860 patients with a history of ischemic stroke or transient ischemic attack were randomized to achieve an LDL-C level below 70 mg/dL (lower-target group) or between 90 and 110 mg/dL (higher-target group).22 The group with the lower LDL-C goal had a 30% lower risk of experiencing a subsequent MACE. Notably, 40% of patients in the lower LDL-C arm received combination therapy with statin plus ezetimibe. Recent data further show that combination therapy, especially fixed-dose combinations, achieves more effectively lipid targets and CV prevention.23,24 In addition, implementing combination therapies from the early stages, or even from the outset, is suggested to increase the number of patients achieving LDL-C goals, thereby preventing new CV events and improving existing atherosclerotic lesions.6
Basing on evidence, international guidelines recommend the use of combination therapy to achieve the ambitious LDL-C goals. Despite this, as previously mentioned, there is a substantial gap between recommendations and routine clinical practice in the management of dyslipidemias. For instance, a retrospective analysis of the Swiss Secondary Prevention Registry (SwissPR) involving 875 patients with coronary artery disease reported that, following the 2019 ESC/EAS guidelines, only 18% of patients were receiving combination therapy with ezetimibe upon entry into cardiac rehabilitation, and 2% were prescribed with PCSK9 inhibitors.25 Barriers contributing to the gap between guidelines recommendations and routine clinical practice may include those related to the physician (i.e. therapeutic inertia or the misperception of attained LDL-C targets), or to the healthcare system (such as restricted access to combination therapy and/or add-on therapies).26,27 Selecting the most appropriate LLT capable of achieving therapeutic targets from the outset often entails the upfront use of combination therapy, rather than relying on the traditional stepwise approach, which remains endorsed by current dyslipidemia management guidelines.5,28 Initiating therapy based on treatment goals may not only facilitate faster attainment of lipid targets but also minimize the therapeutic inertia.
In our SANTORINI Spain cohort, the increase in LLT usage led to a decrease in LDL-C levels in both patients at high and very high risk. Consequently, the percentage of patients who achieved LLT goals also increased in the same period of time. Interestingly, patients who especially improved the LDL-C control were those who were not receiving LLT at baseline (from 8.6% to 32.4%). In contrast, patients who were receiving LLTs at baseline showed a more modest improvement in LDL-C control, which was observed only in those who changed to combination therapy. Despite of this, in our study, LLT during the 1-year follow-up was unchanged in most of the patients (73.1%). This observation aligns with previous studies, showing that LLT optimization often involves only statin dose escalation.6,7,16 Interestingly, in a Czech study evaluating the adherence of cardiologists to guidelines, authors showed that, in up to 61.5% of the patients at very high CV risk who failed to reach their LDL-C targets, their cardiologists expressed satisfaction with the therapeutic outcomes and chose not to change the treatment.7
When comparing to SANTORINI Europe,16 the overall percentage of patients achieving LDL-C targets after 1-year of follow-up was numerically higher in Spain (34.1% versus 30.4% in Europe). However, in Spain it was lower in patients at high risk (27.3% versus 31.6%) but higher in those at very high risk (37.0% versus 30.0%). The lower achievement of targets in patients at high risk in Spain contrasts with the fact that a greater percentage of patients at high risk in Spain were using combination therapy. This observation could be attributed to a higher percentage of patients included with familial hypercholesterolemia in Spain, 15.4% versus 10.4% in Europe, or possibly due to differences in the CV risk classification between Spain and Europe.16
One limitation of the study may derive from the potential selection bias inherent in observational studies. Participating sites, frequently more experienced, might show a best-case scenario. Additionally, the 50% reduction in LDL-C from baseline was not considered for evaluating the attainment for LDL-C goals. Given the non-interventional nature of the study, no formal hypotheses were tested; thus, conclusions should be cautiously made. Despite these limitations, this is the first prospective study that provides an up-to-date picture of the lipid management and LDL-C goal attainment in patients at highest CV risk in Spain after the 2019 update of the ESC/EAS guidelines. In addition, it presents data on a large cohort of patients with available LDL-C levels from both baseline and 1-year follow-up.
ConclusionData of 1-year follow-up from SANTORINI Spain show that the LLT usage increased from baseline, including both monotherapy and combination therapy. Despite recommendations, patients at highest CV risk continue not receiving the most adequate LLT for reducing their LDL-C levels in routine clinical practice. Future dyslipidemia management guidelines should recommend tailoring initial LLT to the magnitude of the LDL-C reduction required, in order to achieve therapeutic goals earlier and reduce therapeutic inertia.
FundingThis study was funded by Daiichi Sankyo Europe GmbH, Munich, Germany. Medical writing assistance was provided by Evidenze Health España S.L.U. and funded by Daiichi Sankyo Europe.
JMM declares having received consultancy fees from Daiichi Sankyo, Novartis, and Sanofi; payments/fees from Daiichi Sankyo, Amgen, Novartis, Servier, Sanofi, Ferrer, and Viatris; and support to attend meetings from Daiichi Sankyo. CL declares consultancy fees from Daiichi Sankyo, Amarin, Alter, Novartis, and Sanofi. MGdYC has served as an advisor or speaker for Daiichi Sankyo. NP declares consultancy fees (as a speaker) from Sanofi, Amgen, and Ferrer. ALC declares having received grants/contracts from Amryt Pharma, Menarini, and Ultragenyx; and payments/fees from Amarin, Amgen, Amryt Pharma, AstraZeneca, Daiichi Sankyo, Esperion, Ionis Pharmaceuticals, Medscape, Menarini, Merck, Novartis, Novo Nordisk, Peervoice, Pfizer, Recordati, Regeneron, Sandoz, Sanofi, The Corpus, Ultragenyx, and Viatris. GDM is an employee of Daiichi Sankyo. KKR declares having received editorial support from Springer funded by Daiichi Sankyo Europe; consultancy from Daiichi for the development of the statistical analysis plan, protocol, and oversight as Principal Investigator; grants/contracts from Amgen, Daiichi Sankyo, Sanofi, Regeneron, and Ultragenyx; consultancy fees from Abbott Laboratories, Amgen, AstraZeneca, Bayer Healthcare Pharmaceuticals, Boehringer Ingelheim, Cargene, CRISPR, Daiichi Sankyo, Eli Lilly Company, EmendoBio, Esperion, Kowa, New Amsterdam Pharma, Novartis Corporation, Nodthera, GSK, Novo Nordisk, Pfizer, Regeneron, Sanofi, SCRIBE, Silence Therapeutics, and VAXXINITY; payments/fees from Novartis, Daiichi Sankyo, Novo Nordisk, Amgen, Sanofi, and Boehringer Ingelheim; and stock options from New Amsterdam Pharma, Scribe, and Pemi31. He is also the President of EAS. JMRC, EV, AIG, JFD, NP, MR-M, JdDG-D, FMD, and IPdP declare no conflicts of interest.
The work of ALC is supported by the Ricerca Corrente grant from the Ministry of Health to Multimedica IRCCS.