El empeoramiento de la función renal es un índice de mal pronóstico en pacientes con insuficiencia cardiaca aguda (ICA). El cociente urea/creatinina (U/C) podría tener significación pronóstica en la ICA.
Material y métodosEstudio observacional, prospectivo, cuyo objetivo fue analizar el valor pronóstico del cociente U/C, determinado en las primeras 24-48h del ingreso, en pacientes hospitalizados por ICA, así como su relación con el filtrado glomerular estimado (FGe) y el daño renal agudo (DRA).
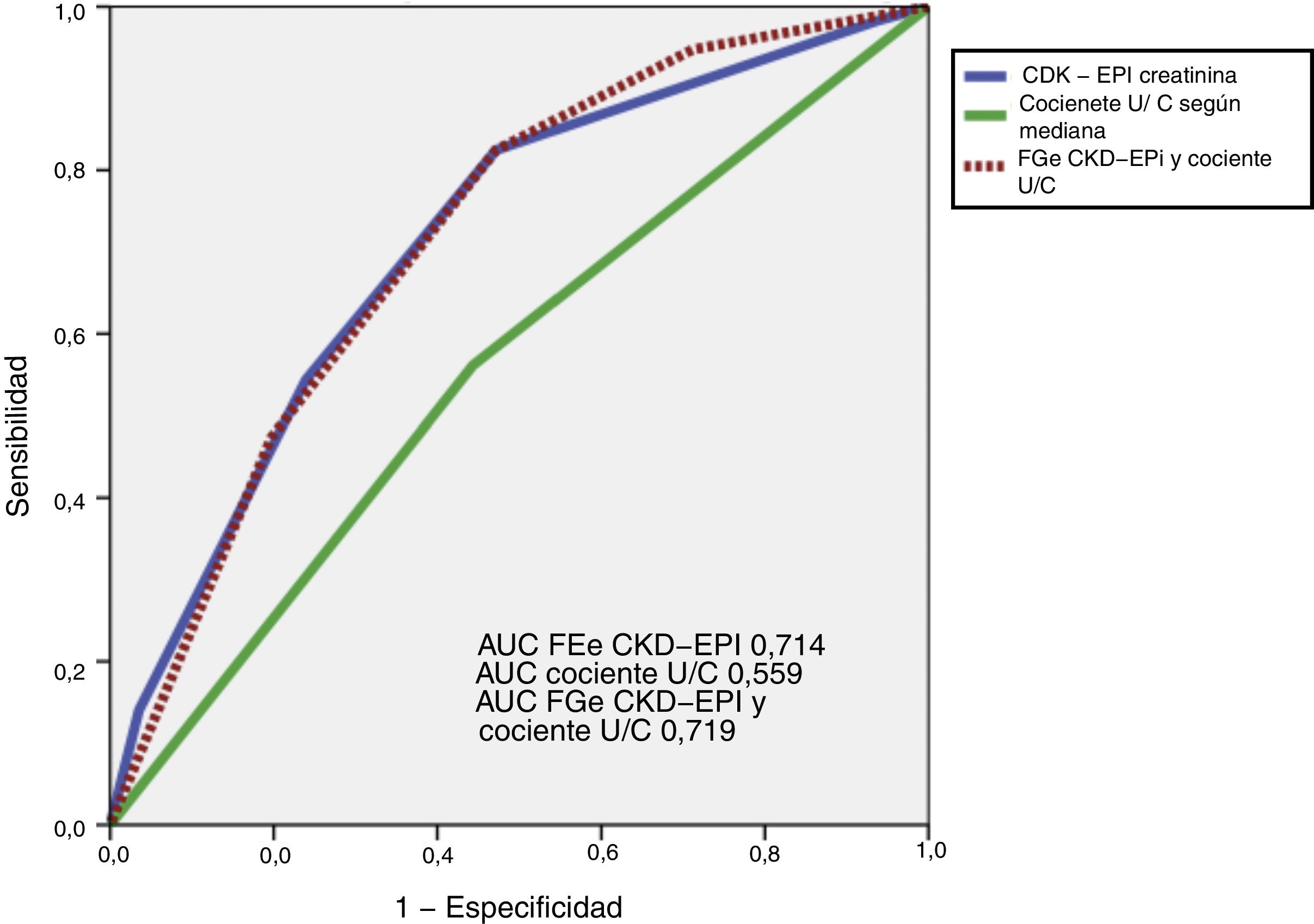
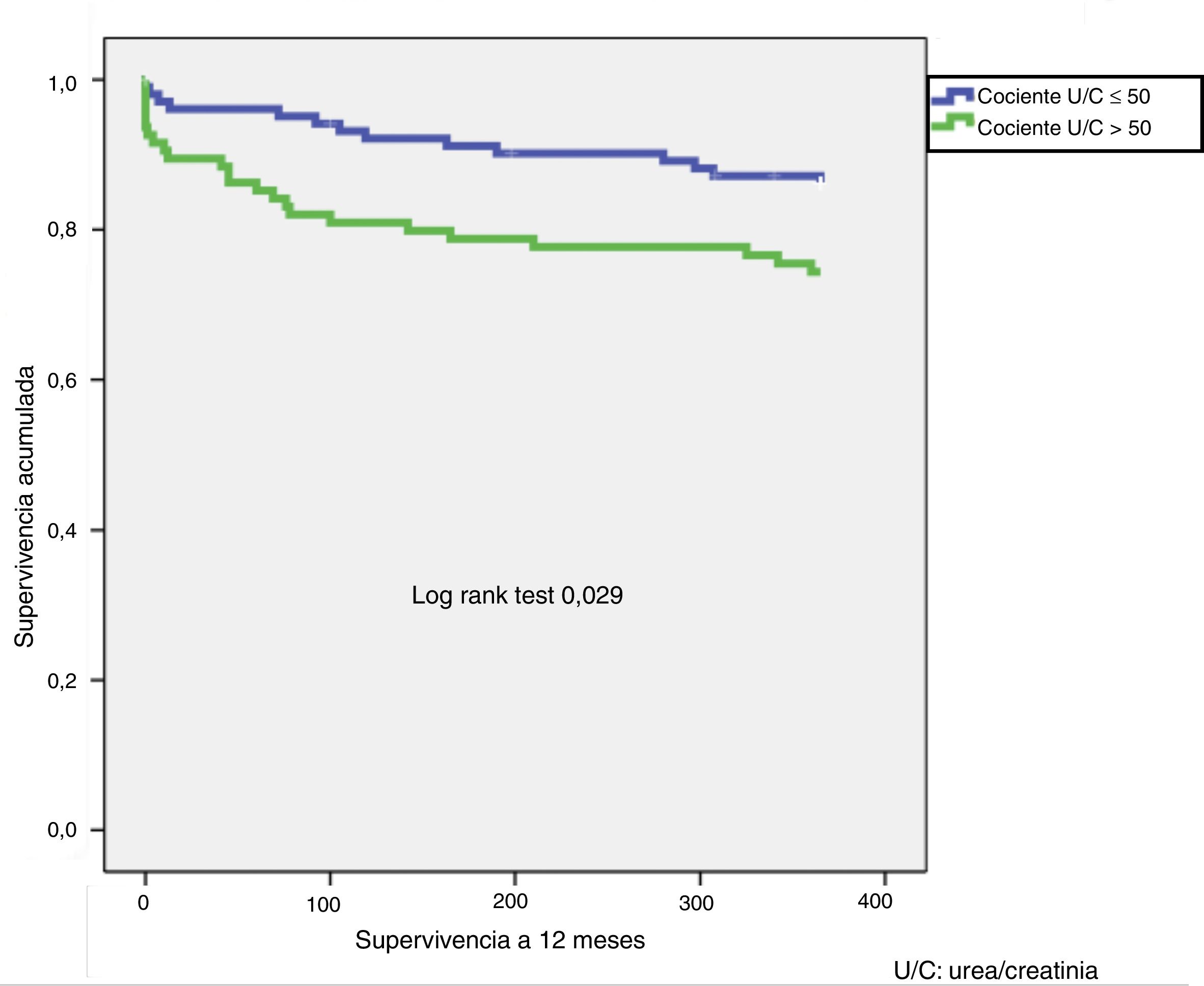
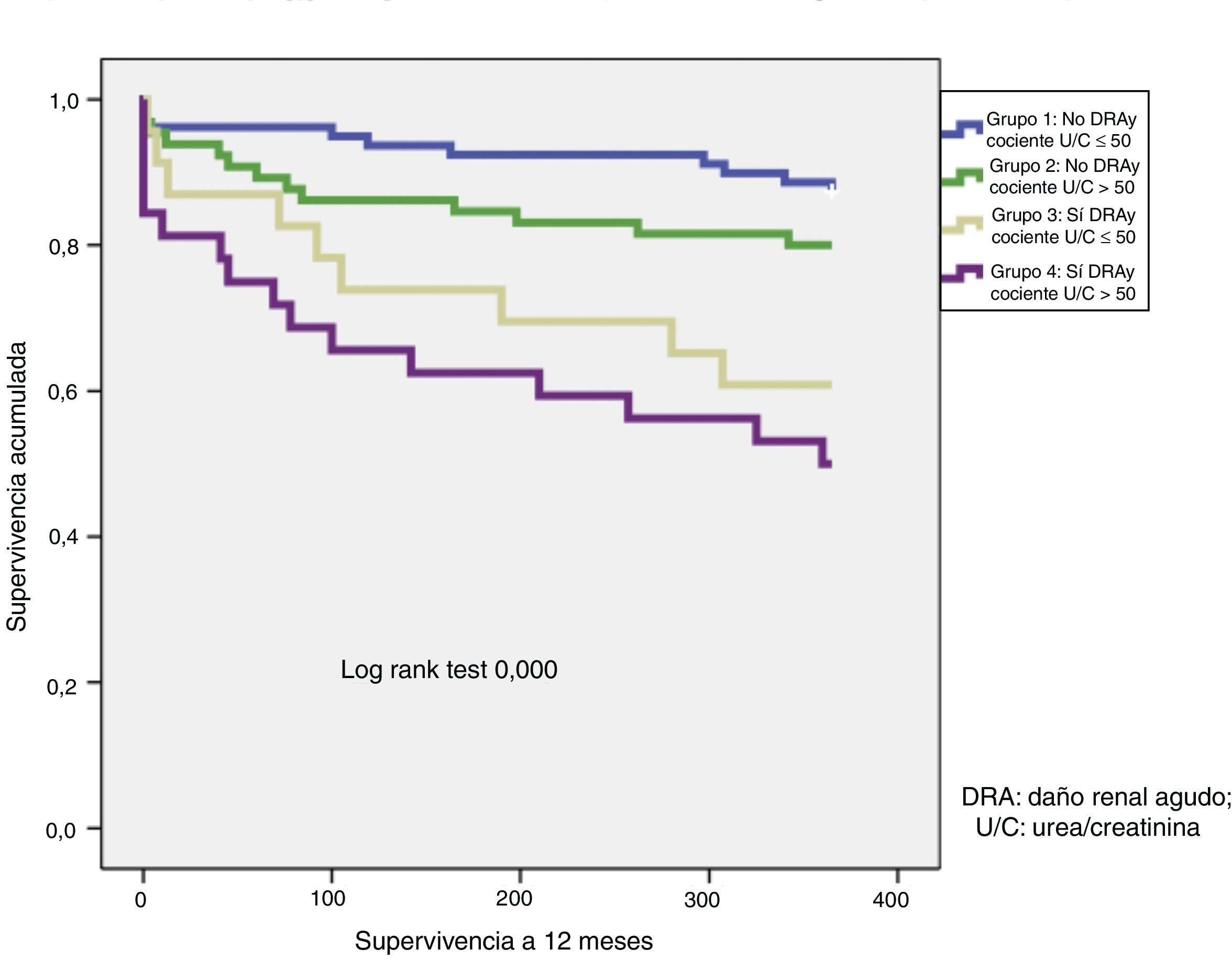
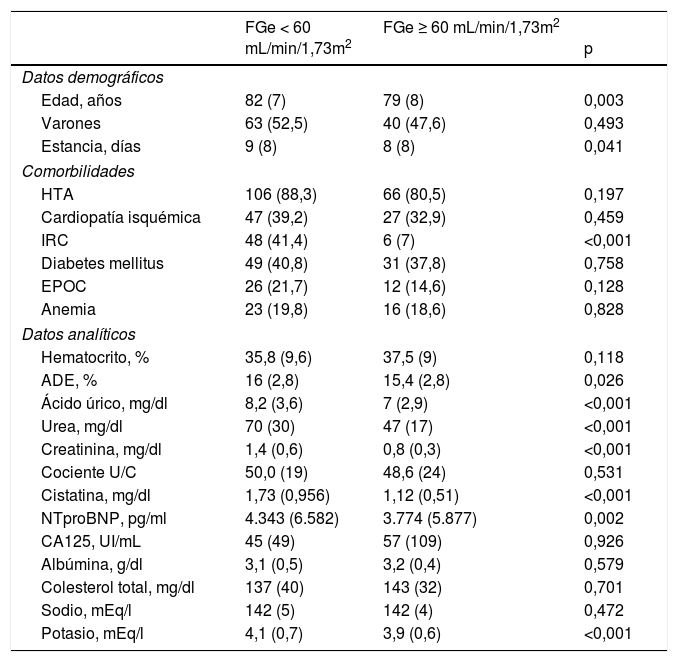
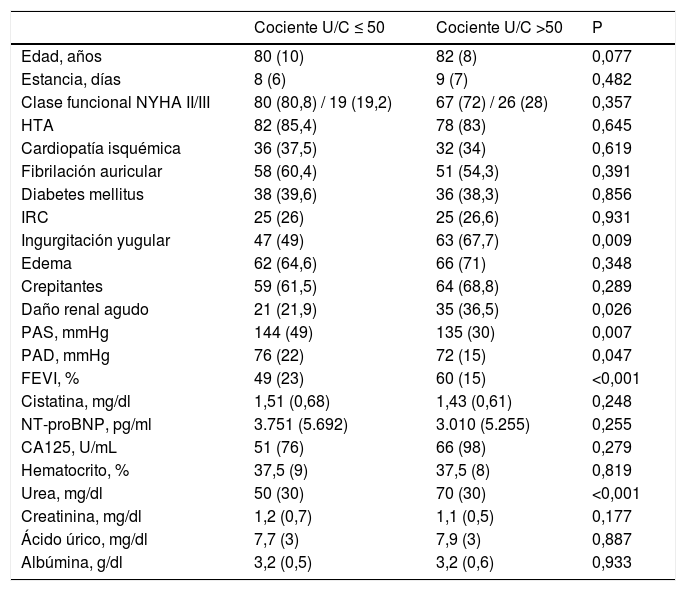
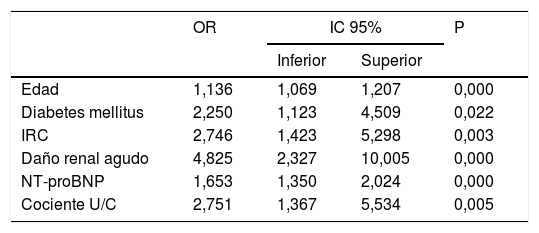
ResultadosSe incluyeron un total de 204 pacientes, con edad media de 79,3 años. La mediana de FGe fue 55ml/min/1,73m2. En el análisis multivariante, un cociente U/C > 50 se asoció con una mayor probabilidad de DRA durante el ingreso (36,5% vs. 21,9%) y mortalidad por cualquier causa (odds ratio [OR] 2,75) y por IC (OR 3,50) durante el seguimiento. La elevación del cociente U/C fue pronóstica solo en los pacientes con FGe normales (mortalidad 4,4% vs. 22%; p=0,01). La combinación del cociente U/C con el FGe tuvo mayor capacidad predictiva de DRA que cada uno de ellos por separado (área bajo la curva 0,718, intervalo de confianza al 95% 0,643-0,793; p<0,001).
ConclusionesUn cociente U/C > 50 predice mortalidad a largo plazo en pacientes con FGe normal, y combinado con el FGe, mejora la identificación del riesgo de DRA, en pacientes ingresados por ICA. Dado lo simple de este biomarcador, sugerimos su uso sistemático en la clínica diaria.
Worsening renal function is associated with an adverse prognosis for patients with acute heart failure (AHF). Urea-creatinine ratio (U:C ratio) might be useful for measuring renal function and could help stratify patients with AHF.
Material and methodsAn observational and prospective study was conducted to analyse the prognostic value of the U:C ratio, measured during the first 24-28 hours of admission, for patients hospitalised for decompensated Heart failure, and its relationship with estimated glomerular filtration rate (eGFR) and acute kidney injury (AKI).
ResultsThe study included 204 patients, with a mean age of 79.3 years, and a median eGFR of 55 mL/min/1.73m2. In the multivariate analysis, an U:C ratio above the median (50) was related to the development of AKI (36.5% vs. 21.9%) and to increased mortality, both overall (OR 2.75) and by HF (OR 3.50) in long term. In combination with eGFR, the U:C ratio showed prognostic value in patients with normal eGFR (mortality of 4.4% for an U:C ratio ≤ 50 vs. 22% for U:C ratio > 50; p=0.01), as well as a better predictive capacity for AKI than each of them separately (AUC, 0.718; 95% CI 0.643-0.793; p>.000).
ConclusionsAn U:C ratio > 50 is a predictor of increased long-term mortality for patients hospitalised for decompensated HF and with normal eGFR. Given the simplicity of this biomarker, its use in clinical practice should be more systematic.
Artículo
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<