This work aims to analyze the impact of Spain’s National Center for Cardiovascular Research (CNIC-Ferrer)’s cardiovascular (CV)-polypill on blood pressure (BP) and low-density lipoprotein cholesterol (cLDL) levels in patients in our healthcare area who previously took equipotent doses of statins and antihypertensives.
Material and methodsAll patients in our healthcare area (Santiago de Compostela, Spain) who, as of December 31, 2019, had an active prescription for the CV-polypill (CNIC-Ferrer) since January 16, 2015 were registered. The index date was the start date of the CV-polypill prescription. The drugs the patient had previously received for dyslipidemia and hypertension were analyzed, classifying them by their equivalent potency to atorvastatin and ramipril. Changes in cLDL and BP were analyzed by means of Student’s t-test for paired samples.
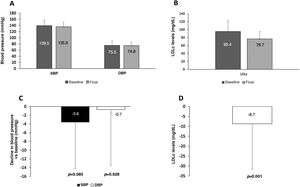
ResultsWe analyzed 547 patients with a mean age of 71.5 ± 11.5 years. The majority were men (60.6%). We observed a decrease in cLDL (−10.6 [95% CI: −7.0, −14.3], p < 0.001) in patients who started taking the CV-polypill who had previously taken equally potent doses of atorvastatin (n = 471). We documented a reduction in systolic BP (−3.7 [95% CI: −0.4, −6.9], p = 0.029) in patients who had previously taken equally potent doses of ramipril (n = 360). In 88 patients, the CV-polypill was started via equally potent doses of atorvastatin and ramipril, with a decrease in cLDL (−8.7 [95% CI: −3.8, −13.6], p = 0.001) and systolic BP (−3.6 [95% CI: −7.8, 0.5], p = 0.085).
ConclusionsThe initiation of treatment with the CV-polypill in patients who previously received equally potent treatment with atorvastatin and ramipril was associated with a greater reduction in cLDL and systolic BP.
Analizar el impacto del inicio del tratamiento con la polipíldora-cardiovascular (CV) del Centro Nacional de Investigaciones Cardiovasculares (CNIC-Ferrer), en las cifras de presión arterial (PA) y colesterol ligado a lipoproteínas de baja densidad (LDL), de los pacientes de nuestra área sanitaria que previamente recibían dosis equipotentes de estatinas y antihipertensivos.
Material y métodosSe registraron todos los pacientes de nuestra área sanitaria (Santiago de Compostela) que a 31 de diciembre de 2019 tenían una prescripción activa de polipíldora-CV (CNIC-Ferrer), desde el 16 de enero de 2015. La fecha índice fue la fecha de inicio de prescripción de polipíldora-CV, y se analizaron los fármacos que previamente recibía el paciente para dislipemia e hipertensión arterial, clasificándose por equipotencias con atorvastatina y ramipril. Se analizó mediante la prueba t-Student para muestras apareadas las variaciones de colesterol LDL y PA.
ResultadosAnalizamos 547 pacientes con una edad media de 71,5 ± 11,5 años y la mayoría varones (60,6%). Observamos un descenso del colesterol LDL (−10,6 [IC95%: −7,0, −14,3], p < 0,001) en los pacientes (n = 471) que iniciaron la polipíldora-CV con dosis previas equipotentes de atorvastatina. Documentamos una reducción de la PA sistólica (−3,7 [IC95%: −0,4, −6,9], p = 0,029) en los pacientes (n = 360) con inicio a partir de dosis equipotentes de ramipril. En 88 pacientes, el inicio de la polipíldora-CV se hizo a partir de dosis equipotentes de atorvastatina y ramipril observándose un descenso del colesterol LDL (−8,7 [IC95%: −3,8, −13,6], p = 0,001) y de la PA sistólica (−3,6 [IC95%: −7,8, 0,5], p = 0,085).
ConclusionesEl inicio del tratamiento con la polipíldora-CV, en pacientes que previamente recibían tratamientos equipotentes de atorvastatina y ramipril, se asoció a una mayor reducción del colesterol LDL y la PA sistólica.
The concept of a polypill arose based on a theoretical estimation which proposed that the combined, simultaneous administration of various drugs indicated for the control of different cardiovascular risk factors (CVRF) could reduce the incidence of cardiovascular (CV) events by 80%.1 Later clinical trials confirmed the efficacy of a polypill in terms of a decline in low-density lipoprotein cholesterol (LDLc) and blood pressure (BP) in both primary2 and secondary prevention.3 Recently, the efficacy of adding acetylsalicylic acid (ASA) to a polypill for a reduction of CV events has been demonstrated.4
One of the arguments in favor of a CV-polypill is improved adherence. In this regard, the FOCUS study, Fixed Dose Combination Drug (Polypill) for Secondary Cardiovascular Prevention, (ASA, simvastatin, and ramipril; CNIC-FS-Ferrer polypill), demonstrated an increase in adherence without observing any significant declines in BP or LDLc.5 Another recent pharmacodynamics clinical trial demonstrated that the CNIC-Ferrer CV-polypill with atorvastatin decreased LDLc figures, but not BP figures, due to a possible synergistic effect among the components.6
The SORS study, a prospective clinical registry in a population in Mexico,7 found that use of the CV-polypill reduced both LDLc8 and BP more than treatment with the separate components.9 However, we do not have real-world data that allow for analyzing its impact on said risk factors in a routine clinical practice setting, comparing it to prior treatment with equally potent doses of statins and antihypertensive drugs.
Given the available evidence, we hypothesize that the CV-polypill could be associated with a greater reduction in BP and LDLc figures in patients who previously received treatment with equally potent doses of statins and antihypertensive drugs.
The aim of our study was to analyze the impact of starting treatment with the CNIC-Ferrer CV-polypill on BP and LDLc figures in patients in our healthcare area who previously received equally potent doses of statins and antihypertensive drugs.
Materials and methodsPatientsThis work is a retrospective observational analysis of all patients who had an active prescription for the CV-polypill from January 2015 to December 2019 in our healthcare area (Santiago de Compostela) based on the prescription section of our electronic medical record.
The study protocol was approved by the Drug Research Ethics Committee of Galicia (DREC-G) with registry code 2021/056.
The variables recorded are listed and defined in Appendix A of the supplementary material.
Outcome variableWe analyzed changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) figures in each visit to the health center and the complete lipid profile (total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDLc) and LDLc) on any blood tests performed.
Any available measurements of both variables in the period from one year before the index date until the end of the observation period were recorded. To express the results, BP or LDLc prior to the use of the CV-polypill were used for comparison, with the last measurement conducted during the previous treatment (Appendix A Figure S1 of the supplementary material).
Statistical analysisThe SPSS 22.0 statistical package for Windows was used for data handling and analysis.
In the descriptive analysis of the sample, the descriptive parameters of the variables were used: mean and standard deviation (SD), median and interquartile range (P25, P75), and percentages. The bivariable analysis of the qualitative variables was conducted using the chi-square test.
To analyze the impact of treatment with the CV-polypill, variations in BP and LDLc figures were analyzed in each patient before and after the treatment. To do so, comparisons were made using Student’s t test for paired samples. The calculations were conducted for the sample as a whole and for various subgroups who received different equally potent doses of ramipril and atorvastatin according to the antihypertensive and lipid-lowering drugs subjects took previously.10–12
All results are expressed to the tenths place and no rounding was performed during the calculations. A p value less than .05 was considered statistically significant.
ResultsDescription of the sampleData on 547 patients were recorded (Table 1). The mean age was 71.5 ± 11.5 years and 60.6% were men. The most prevalent CVRF was HT, 2.1% of patients had prior CV disease, and 19.7% met criteria for chronic kidney disease (CKD). The median follow-up time for the sample was 55 (15, 118) months.
Baseline characteristics in all patients and according to the CV-polypill composition.
| According to the CV-polypill composition | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total | AT 20 mg | AT 40 mg | p | RAM 2.5 mg | RAM 5 mg | RAM 10 mg | p | |
| (n = 547) | (n = 379) | (n = 168) | (n = 173) | (n = 176) | (n = 198) | |||
| Sex (female), n (%) | 218 (39.4) | 166 (44.0) | 50 (29.8) | 0.002 | 52 (30.1) | 67 (38.1) | 98 (49.5) | <0.001 |
| Age (years), (mean ± SD) | 71.5 ± 11.5 | 72.5 ± 11.2 | 69.3 ± 11.8 | 0.004 | 70.6 ± 13.3 | 71.8 ± 10.6 | 72.2 ± 10.3 | 0.373 |
| Family history of CV disease, n (%) | 27 (5.0) | 11 (3.0) | 16 (9.6) | 0.001 | 9 (5.2) | 9 (4.6) | 10 (5.1) | 0.962 |
| Obesity, n (%) | 225 (41.8) | 11 (3.0) | 16 (9.6) | 0.001 | 63 (36.6) | 75 (42.6) | 90 (45.5) | 0.223 |
| Hypercholesterolemia, n (%) | 473 (86.3) | 163 (42.7) | 65 (38.7) | 0.378 | 144 (83.2) | 159 (90.3) | 169 (85.4) | 0.139 |
| Hypertension, n (%) | 485 (88.5) | 334 (88.0) | 138 (82.1) | 0.067 | 136 (78.6) | 162 (92.0) | 186 (93.9) | 0.000 |
| Diabetes mellitus, n (%) | 229 (41.8) | 162 (42.7) | 67 (39.9) | 0.531 | 68 (39.3) | 74 (42.0) | 87 (43.9) | 0.664 |
| Prior CV disease, n (%) | 11 (2.1) | 8 (2.2) | 3 (1.8) | 0.796 | 2 (1.2) | 5 (2.9) | 4 (2.1) | 0.540 |
| Heart failure, n (%) | 42 (7.7) | 163 (42.9) | 67 (39.9) | 0.505 | 68 (39.3) | 74 (42.0) | 87 (43.9) | 0.664 |
| Chronic kidney disease, n (%) | 108 (19.7) | 29 (7.7) | 13 (7.7) | 0.998 | 12 (6.9) | 17 (9.7) | 13 (6.6) | 0.483 |
| Atrial fibrillation, n (%) | 15 (2.7) | 75 (19.7) | 33 (19.6) | 0.980 | 49 (28.3) | 25 (14.2) | 34 (17.2) | 0.002 |
| BMI (kg/m2; mean ± SD) | 30.6 ± 5.2 | 30.7 ± 5.4 | 30.2 ± 4.6 | 0.311 | 30.2 ± 5.0 | 30.4 ± 4.7 | 30.9 ± 5.6 | 0.546 |
| SBP (mmHg) (mean ± SD) | 142.7 ± 18.4 | 144.9 ± 18.2 | 137.4 ± 17.5 | <0.001 | 140.8 ± 19.8 | 142 ± 17.9 | 144.7 ± 17.4 | 0.172 |
| DBP (mmHg) (mean ± SD) | 79.2 ± 12.1 | 80.4 ± 11.7 | 76.3 ± 12.5 | 0.001 | 77.7 ± 12.6 | 79.0 ± 12.3 | 80.4 ± 11.4 | 0.164 |
| Total cholesterol (mg/dL), (mean ± SD) | 176.1 ± 80.2 | 182.2 ± 93.0 | 163.2 ± 38.3 | 0.001 | 173.9 ± 49.2 | 171.9 ± 43.4 | 182.0 ± 119.0 | 0.446 |
| Triglycerides (mg/dL), (mean ± SD) | 131.9 ± 73.4 | 128.3 ± 73.0 | 140.4 ± 74.7 | 0.081 | 135.6 ± 83.1 | 135.9 ± 75.9 | 124.9 ± 61.1 | 0.269 |
| HDL cholesterol (mg/dL), (mean ± SD) | 48.2 ± 16.6 | 50.0 ± 18.1 | 44.3 ± 12.0 | <0.001 | 47.2 ± 14.2 | 48 ± 15.8 | 49.2 ± 19.1 | 0.532 |
| LDL cholesterol (mg/dL), (mean ± SD) | 98.8 ± 35.6 | 102.7 ± 37.0 | 90.48 ± 31.1 | <0.001 | 99.4 ± 40.1 | 96.3 ± 33.3 | 100.6 ± 33.2 | 0.528 |
Quantitative variables are shown as mean ± SD. Qualitative variables are shown as total number of patients (n) and percentage of the total sample.
AT: atorvastatin; BMI: body mass index; CV disease: cardiovascular disease; DBP: diastolic blood pressure; DM: diabetes mellitus; HDL: high-density lipoprotein cholesterol; HT: hypertension; LDL cholesterol: low-density lipoprotein cholesterol; SBP: systolic blood pressure; SD: standard deviation; RAM: ramipril.
Appendix A Figure S2 of the supplementary material shows the lipid-lowering drugs (A) and antihypertensive drugs (B) prescribed prior to starting the CV-polypill. In addition, 68.5% were in treatment with ASA.
The CV-polypill was started by primary care physicians in 79.3% of cases, followed by cardiologists (6.2%) and neurologists (2.9%).
The mean decline in SBP and DBP and the changes in the lipid profile in the total sample are shown in Appendix A Figure S3 of the supplementary material.
Equal potency to ramipril in the CV-polypillTable 1 shows the baseline characteristics of the patients in whom each of the doses of ramipril were prescribed to. This drug was mostly prescribed to patients with equally potent doses as the individual component: ramipril 2.5 mg (n = 84; 48.6%), ramipril 5 mg (n = 77; 43.8%), and ramipril 10 mg (n = 62; 31.3%).
The use of diuretics was similar among the three ramipril dose groups (28.0% vs. 20.7% vs. 27.4%, respectively, p = 0.218), as was use of beta blockers (32.9% vs. 28.3% vs. 31.3%, respectively, p = 0.341). Calcium channel blockers were most often used in association with the 10 mg ramipril dose (14.0% vs. 17.0% vs. 30.5%, respectively, p < 0.001).
The start of treatment with ramipril 2.5 mg was associated with significant declines in SBP (p < 0.001) and DBP (p = 0.004). The 10 mg dose was also associated with a significant decline in SBP (p < 0.001). The declines observed with the 5 mg dose were not statistically significant (Appendix A Figure S4 of the supplementary material). In cases in which the change to ramipril was from other equally potent molecules, a decline of 3.7 mmHg in SBP was observed (p = 0.029) (Fig. 1).
Equal potency to atorvastatin in the CV-polypillTable 1 shows the baseline characteristics of patients according to the dose of atorvastatin in the CV-polypill. It was mostly started in patients treated with statins that were equally potent to atorvastatin 20 mg (n = 328; 59.4%) and atorvastatin 40 mg (n = 143; 66.1%). The start of treatment with the polypill that contained atorvastatin 20 mg or 40 mg was associated with a significant decrease in LDLc (p = 0.005 and p < 0.001, respectively) (Appendix A Figure S3 of the supplementary material).
In cases in which the statin in the CV-polypill was changed from another equally potent statin, we observed a mean decline in LDLc of 10.6 mg/dL (p < 0.001) (Fig. 2).
In cases in which a change was made simultaneously to equally potent doses of ramipril and atorvastatin (n = 88), a decline of 8.7 mg/dL in LDLc was observed (p = 0.001); the decline in BP was not statistically significant (Fig. 3).
DiscussionThe results of our study show that in routine clinical practice, a significant reduction in LDLc and SBP is observed in patients who start treatment with the CV-polypill compared to previous values under treatment with equally potent doses of statins and antihypertensive drugs.
Our findings could be justified by greater treatment adherence by substituting the individual components for the CV-polypill and a possible synergistic effect among the polypill’s components.5–7,13,14
To our knowledge, this is the first time that efficacy of the CV-polypill in routine clinical practice has been described in terms of lipid and BP control compared to the individual components of equally potent drugs. It could provide additional information to what has been reported in clinical trials or prospective registries.7 We believe that our findings have certain clinical implications for the optimization of cardiovascular risk factor control (LDLc and BP) and secondary prevention in patients with ischemic heart disease.
Various publications have described greater treatment compliance with polypills compared to treatment with individual components. However, the results are not uniform when its efficacy is assessed by means of LDLc and BP control. In the FOCUS study, the greater treatment adherence described was not accompanied by a significant reduction in LDLc or BP levels in the group of patients which received the polypill compared to those treated with individual components.5 The authors stated that the lack of better control despite a significant increase in treatment compliance could be due to various reasons, including the characteristics of the clinical trial’s design with a polypill that included simvastatin.
The SORS study7 evaluated clinical efficacy (in terms of a reduction in BP and lipids) in a heterogeneous group of patients (secondary prevention and patients with high and moderate cardiovascular risk) who received the CV-polypill in real-world clinical practice in Mexico. In addition to their habitual treatment, patients received a polypill which contained 100 mg of aspirin, 5 or 10 mg of ramipril, and 40 mg of simvastatin for one year. A significant reduction in BP, total cholesterol, and LDLc levels was observed, but no changes were observed in HDLc. In particular, the decrease of 26.3 mg/dL in mean LDLc from a mean of 137.3 mg/dL should be noted.
The difference observed in our study could be due to the lower baseline LDLc levels in our patients, with an initial level of 102.4 mg/dL among those who were prescribed the 20 mg dose of atorvastatin and 90.5 mg/dL among those treated with 40 mg.
In our setting, the results of our analysis complement the clinical aspects associated with treatment with the CV-polypill, as they include all patients treated with this strategy in real-world clinical practice conditions in a healthcare area.
Additionally, we evaluated efficacy in terms of a reduction in BP and lipid levels in patients treated with antihypertensive and lipid-lowering drugs with a similar potency to the CV-polypill components. This allowed us to determine their real incremental effect compared to treatment with the individual components.
As we stated, to our knowledge, this is the first time a study of these characteristics has been conducted. It could strengthen the role of polypills, such as the one studied, in achieving better cardiovascular prevention. The greater efficacy of the CV-polypill in the reduction of BP and LDLc could be related not only to better treatment compliance, but also to a possible synergistic effect of the joint administration of the drugs that it is composed of.
In a recent clinical study, a greater reduction in BP figures, as measured by outpatient monitoring, and LDLc was observed in a group of patients randomized to receive the CV-polypill compared to those treated with the individual components (ramipril and atorvastatin), although only the LDLc reduction was statistically significant.6 Specifically, an additional 7% reduction in LDLc was observed, similar to what was described when the statin dose was doubled.
The lack of differences in treatment compliance in patients among the trial’s three arms ruled out its influence on the results and suggested the possibility of synergies among statins and ACE inhibitors.
Lastly, the high rate of aspirin use in our patients should be mentioned, given that less than 10% had prior CV disease. Low rates of recording cardiovascular disease in the medical records or the decision to provide antiplatelet drugs to patients according to their elevated CV risk could have influenced this finding.
The recent results of the POLYCAP 3 study with another polypill (simvastatin, atenolol, hydrochlorothiazide, and ramipril) associated with ASA or not in patients with intermediate risk show that combined treatment with aspirin was related to a significant reduction in CV events.4
Limitations of the studyThis retrospective study analyzes the clinical characteristics included in the comprehensive electronic medical record of patients treated with the CV-polypill in our healthcare area. It has the limitations inherent to this type of design, in which BP measurements and drug prescribing are carried out in a routine clinical practice setting.
However, we believe that these characteristics may also be a strength, as there are no conditioning factors in the patients’ clinical evaluation, including the measurement of BP figures or the frequency of analytical tests. In addition, evaluating the changes in light of the equal potency of the CV-polypill to previous treatment with the individual components strengthens the hypothesis of a net synergistic effect exerted by the polypill.
We did not have all variables for all patients, as it was dependent on them being recorded on the medical record. However, the percentage of missing values per variable was 0.07%, a fact that strengthens the validity of our findings. Along these lines, the availability of information such as adjuvant treatments and the evolution of BP measurements and LDLc analyses are sufficiently abundant for analyzing the evolution of the main variables and controlling for the effect of confounding factors.
We are aware that assuming the equal potency of antihypertensive drugs and statins with ramipril and atorvastatin in the CV-polypill has certain limitations; however, they are those recommended by clinical practice guidelines and reference meta-analyses.10–12
Finally, we do not know the indication of the CV-polypill and we were not able to evaluate patients’ treatment compliance either during the period in which they were treated with the individual components or with the CV-polypill, which are aspects that could influence our results.
ConclusionsInitiating treatment with the CV-polypill was associated with a significant decline in LDLc and BP figures. Among patients who had previously received equally potent treatment with statins and antihypertensive drugs, starting the CV-polypill was associated with a considerable decline in LDLc, but the decline was not statistically significant in the case of SBP.
As we have described, our findings suggest that in a routine clinical practice scenario, the observations of clinical trials and prospective registries which indicate that these effects could be associated with better treatment compliance and a possible synergistic effect among the drugs.
FundingThe authors have not received any funding for the conduct of this study.
Conflicts of interestThe authors declare no conflicts of interest in regard to this article.
Please cite this article as: Portela-Romero M, Cinza-Sanjurjo S, Conde-Sabarís P, Rodríguez-Mañero M, Mazón-Ramos P, Rey-Aldana D, et al. Efecto en la vida real sobre el control de los factores de riesgo asociado al inicio con polipíldora cardiovascular a partir de fármacos equipotentes. Rev Clin Esp. 2022;222:131–137.