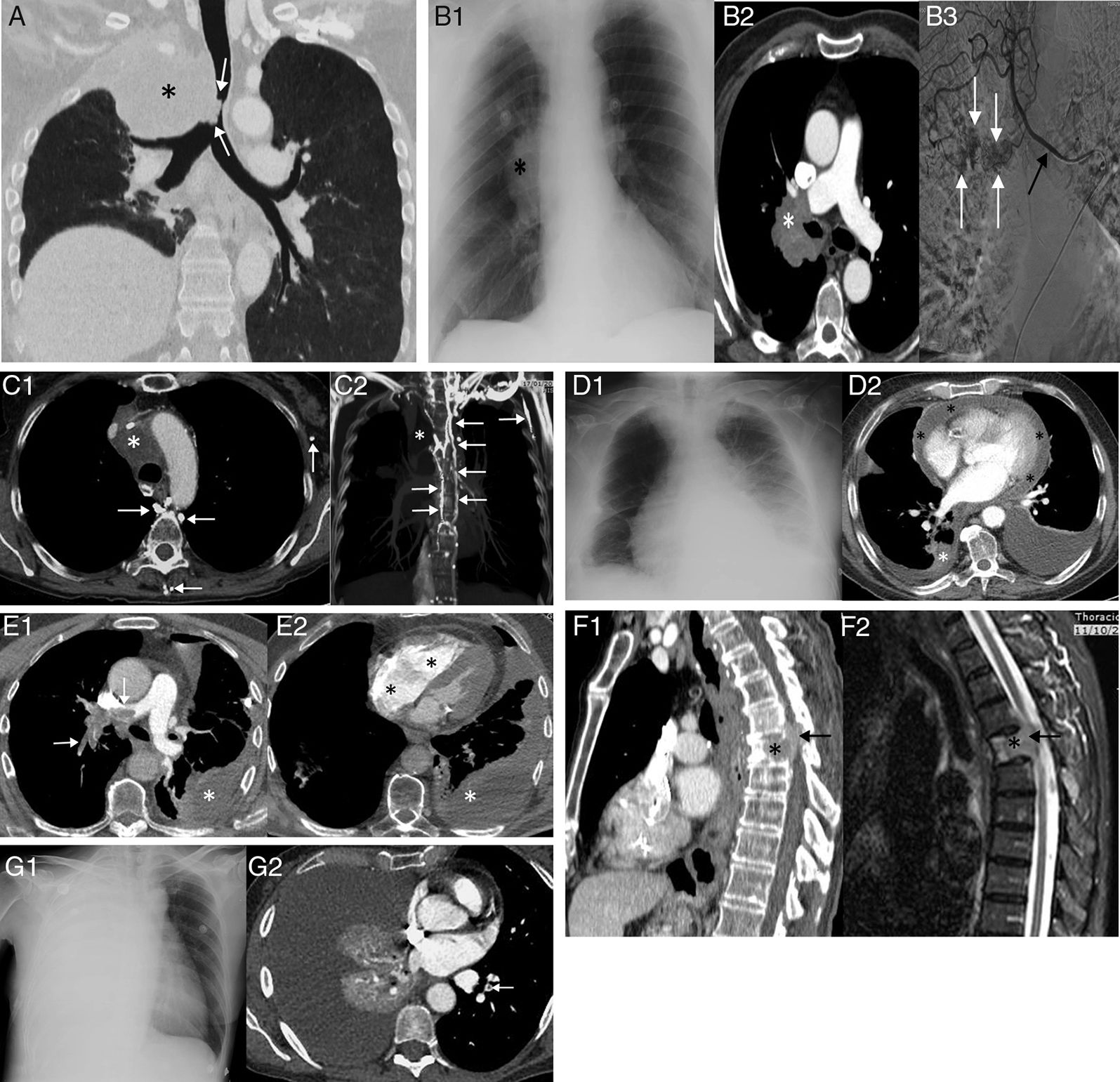
Patients with lung cancer are the type of cancer patient who are most often admitted to emergency departments due to disease-related complications. An oncologic emergency is defined as any acute event in a patient with cancer that develops directly or indirectly from the tumor and that threatens the patient's life. Oncologic emergencies are divided into metabolic, haematologic and structural emergencies. In this article, we address the main structural thoracic complications of patients with lung cancer, in which imaging tests play an essential role in their diagnosis. The main oncologic thoracic emergencies of lung cancer are airway obstruction, superior vena cava syndrome, acute pulmonary thromboembolism, pericardial tamponade, massive haemoptysis, spinal cord compression and pleural effusion. Oncologic emergencies are a significant cause of morbidity and mortality in patients with lung cancer. Emergency department physicians play a fundamental role in the early detection of these emergencies. The knowledge and correct identification of the main oncologic thoracic emergencies of patients with lung cancer therefore enable optimal diagnostic and therapeutic management.
El paciente con cáncer de pulmón es el paciente oncológico que más frecuentemente acude a urgencias por complicaciones relacionadas con su enfermedad. Se define como emergencia oncológica cualquier evento agudo en un paciente oncológico que se desarrolla de manera directa o indirecta debido al tumor y que pone en riesgo la vida del paciente. Las emergencias oncológicas se dividen en metabólicas, hematológicas y estructurales; en este artículo abordaremos las principales complicaciones estructurales torácicas de los pacientes con cáncer de pulmón, en las que las pruebas de imagen tienen un papel fundamental en su diagnóstico. Las principales emergencias oncológicas torácicas del cáncer de pulmón son: obstrucción de la vía aérea, síndrome de vena cava superior, tromboembolismo pulmonar agudo, taponamiento pericárdico, hemoptisis masiva, compresión medular y derrame pleural. Las emergencias oncológicas son causa importante de morbimortalidad en pacientes con cáncer de pulmón. Los médicos de urgencias juegan un papel fundamental en su detección precoz, por lo que el conocimiento y la correcta identificación de las principales emergencias oncológicas torácicas del paciente con cáncer de pulmón permiten un manejo diagnóstico y terapéutico óptimo.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<