This study aims to describe the characteristics of patients with COVID-19 in a state in northern Mexico and establish the comorbidities associated with mortality.
MethodsPatients with COVID-19, divided into survivors and non-survivors, were analyzed. The data were analyzed using the chi-square test, Student’s t-test, and Cox’s regression model.
ResultsA total of 17,479 patients were included and mortality rate of 6.3% was reported. Age over 60 years (HR = 8.04; 95%CI 7.03–9.19), diabetes (HR = 1.63; 95%CI 1.40–1.89), high blood pressure (HR = 1.48; 95%CI 1.28–1.72), obesity (HR = 1.37; 95%CI 1.18–1.60) and chronic kidney disease (HR = 2.06; 95%CI 1.64–2.59) were significantly associated with mortality.
ConclusionsDiabetes, high blood pressure, obesity, and chronic kidney disease increased mortality among patients with COVID-19 in the population of Coahuila, Mexico. The factor that most contributed to risk of death was age over 60 years.
El objetivo de este estudio es describir las características de los pacientes con COVID-19 en un estado del norte de México y determinar las comorbilidades asociadas con la mortalidad.
MétodosSe examinaron pacientes con COVID-19, divididos en supervivientes y no supervivientes. Los datos fueron analizados mediante las pruebas de X2, t de Student y el modelo de regresión de Cox.
ResultadosSe incluyeron 17.479 pacientes, reportando un 6,3% de mortalidad. Los factores que se asociaron con esta fueron: edad mayor a 60 años (HR = 8,04; IC 95% 7,03 a 9,19), diabetes (HR = 1,63; IC 95% 1,40 a 1,89), hipertensión arterial sistémica (HR = 1,48; IC 95% 1,28 a 1,72), obesidad (HR = 1,37; IC 95% 1,18 a 1,60) y daño renal crónico (HR = 2,06; IC 95% 1,64 a 2,59).
ConclusionesLa diabetes, la hipertensión arterial, la obesidad y el daño renal crónico incrementan la mortalidad en pacientes con COVID-19 en la población de Coahuila, México; el factor que más contribuye para el riesgo de muerte es la edad mayor a 60 años.
In December 2019, the World Health Organization (WHO) reported the presence of cases of pneumonia of unknown origin detected in the city of Wuhan, China. The authorities later identified a novel coronavirus (SARS-CoV-2) as the causal agent of this disease (COVID-19)1. The WHO declared this illness to be a global public health emergency on January 30, 2020 and the first case was reported in Latin America approximately one month later2.
The first person with COVID-19 in Mexico was detected on February 27 of that year. Two days later, the state of Coahuila reported its first case of SARS-CoV-2 infection (the fourth in Mexico). On March 30, a healthcare emergency was declared in the country3.
The high rates of hypertension, obesity, and diabetes in Mexico are worrying; it has been demonstrated that the presence of comorbidities associated with SARS-CoV-2 infection increases the risk of mortality. However, the majority of the evidence comes from studies conducted in Asia and thus other investigations that analyze these data in other regions are necessary4,5.
The aim of this study is to describe the characteristics of patients with COVID-19 in a state in Northern Mexico and determine the comorbidities associated with mortality for the purpose of implementing better measures aimed at safeguarding the at-risk population.
MethodsThis work is a retrospective cohort study. The data were obtained from the Respiratory Diseases Surveillance System (SISVER, for its initials in Spanish) platform in the National Epidemiological Surveillance System (SINAVE, for its initials in Spanish) of the General Directorate of Epidemiology of Secretariat of Health of Mexico. This study was approved by the research ethics committee and no data that could identify patients on an individual level were used.
The study included patients from the state of Coahuila de Zaragoza (Mexico) with a positive result for SARS-CoV-2 on a real-time polymerase chain reaction test recorded from March 17 to August 12, 2020.
The real-time polymerase chain reaction test was performed in patients who met the operational definition of a suspected case of COVID-19: “a person of any age who, in the last ten days, has presented with at least one of the following symptoms: cough, dyspnea, fever, or headache accompanied by at least one of the following signs or symptoms: myalgia, arthralgia, odynophagia, chills, chest pain, rhinorrhea, polypnea, anosmia, dysgeusia, or conjunctivitis.” This definition is included in the standard guidelines for epidemiological surveillance and viral respiratory disease laboratory of the Secretary of State of Mexico6.
The statistical analysis considered age, sex, need for in-hospital treatment, requirement for the administration of supplemental oxygen, reported symptoms (fever, cough, rhinorrhea, sore throat, conjunctivitis, anosmia, headache, diarrheal stools, vomiting, abdominal pain, myalgia, arthralgia, overall condition, chest pain, dyspnea, and cyanosis) as well as associated comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, asthma, systemic hypertension, heart disease, obesity, chronic kidney disease, tobacco use, and human immunodeficiency virus infection).
The outcome variable analyzed was mortality. As such, patients were divided into two groups: survivors and nonsurvivors.
The quantitative data were expressed as means and standard deviations. The qualitative variables were expressed as frequencies and percentages. The chi square test and independent Student’s t-test were used to compare the groups.
To determine the risk factors for mortality, age and associated comorbidities were taken into account by means of a univariate and multivariate Cox regression model. Values of p < .05 were considered statistically significant.
The IBM SSPS Statistics program was used for statistical analysis (IBM Corp. Released in 2013. IBM. SPSS Statistics for Windows, Version 21.0. Armonk NY: IBM Corp.).
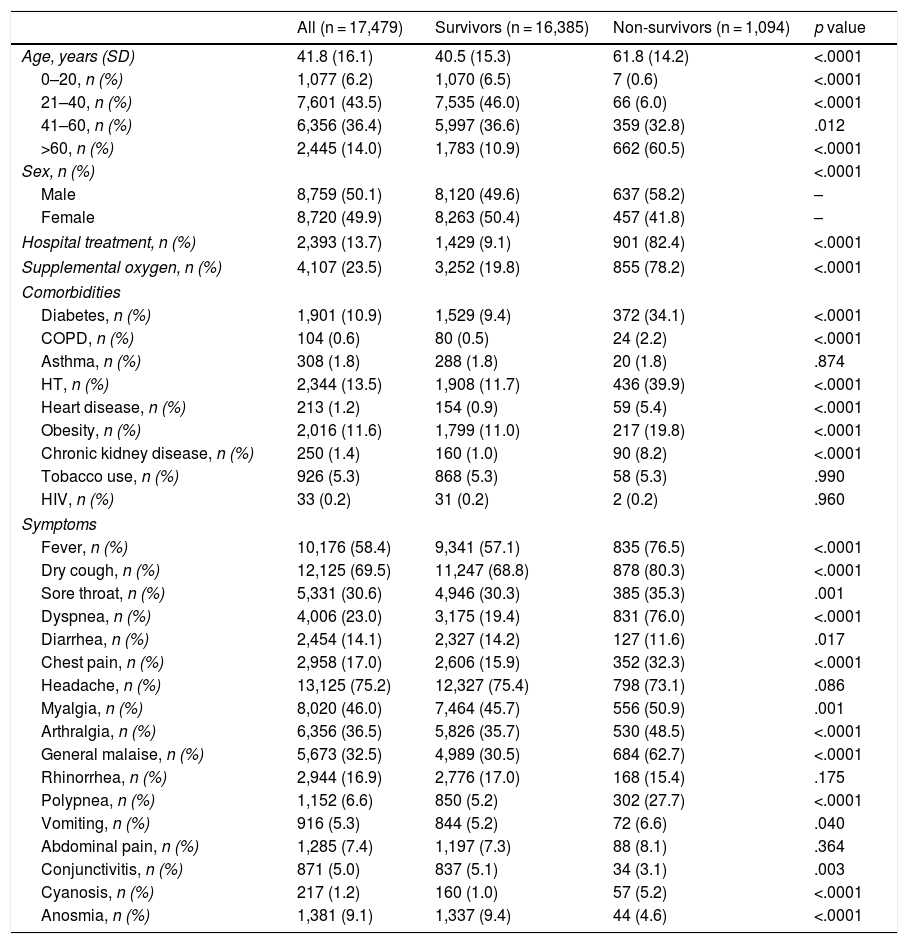
ResultsA total of 17,479 patients were included in the study, of which 8,720 were women (49.9%) and 8,759 were men (50.1%) with a mean age of 41.8 years. Of the total, 13.7% required in-hospital treatment; 23.5% of all participants needed the administration of supplemental oxygen.
The reported mortality was 6.3% (1,094 patients) and 60.5% of those were patients older than 60 years.
The most common symptoms were headache (75.2%) dry cough (69.5%), and fever (58.4%); 23% presented with dyspnea and 1.2% with cyanosis. Systemic hypertension, obesity, and diabetes mellitus were the most frequently reported comorbidities: 13.5%; 11.6%, and 10.9%, respectively.
Age, need for in-hospital treatment, and requirement for supplementary oxygen showed significant differences when comparing survivors versus nonsurvivors (p < .0001).
In the nonsurvivor group, 34.1% presented with diabetes mellitus, 39.9% with systemic hypertension, and 19.8% with obesity vs. 9.4%, 11.7%, and 11%, respectively, in the survivor group (p < .0001).
The rest of the characteristics of the general population as well as the comparisons between groups are shown in Table 1.
Characteristics of patients with COVID-19.
| All (n = 17,479) | Survivors (n = 16,385) | Non-survivors (n = 1,094) | p value | |
|---|---|---|---|---|
| Age, years (SD) | 41.8 (16.1) | 40.5 (15.3) | 61.8 (14.2) | <.0001 |
| 0–20, n (%) | 1,077 (6.2) | 1,070 (6.5) | 7 (0.6) | <.0001 |
| 21–40, n (%) | 7,601 (43.5) | 7,535 (46.0) | 66 (6.0) | <.0001 |
| 41–60, n (%) | 6,356 (36.4) | 5,997 (36.6) | 359 (32.8) | .012 |
| >60, n (%) | 2,445 (14.0) | 1,783 (10.9) | 662 (60.5) | <.0001 |
| Sex, n (%) | <.0001 | |||
| Male | 8,759 (50.1) | 8,120 (49.6) | 637 (58.2) | – |
| Female | 8,720 (49.9) | 8,263 (50.4) | 457 (41.8) | – |
| Hospital treatment, n (%) | 2,393 (13.7) | 1,429 (9.1) | 901 (82.4) | <.0001 |
| Supplemental oxygen, n (%) | 4,107 (23.5) | 3,252 (19.8) | 855 (78.2) | <.0001 |
| Comorbidities | ||||
| Diabetes, n (%) | 1,901 (10.9) | 1,529 (9.4) | 372 (34.1) | <.0001 |
| COPD, n (%) | 104 (0.6) | 80 (0.5) | 24 (2.2) | <.0001 |
| Asthma, n (%) | 308 (1.8) | 288 (1.8) | 20 (1.8) | .874 |
| HT, n (%) | 2,344 (13.5) | 1,908 (11.7) | 436 (39.9) | <.0001 |
| Heart disease, n (%) | 213 (1.2) | 154 (0.9) | 59 (5.4) | <.0001 |
| Obesity, n (%) | 2,016 (11.6) | 1,799 (11.0) | 217 (19.8) | <.0001 |
| Chronic kidney disease, n (%) | 250 (1.4) | 160 (1.0) | 90 (8.2) | <.0001 |
| Tobacco use, n (%) | 926 (5.3) | 868 (5.3) | 58 (5.3) | .990 |
| HIV, n (%) | 33 (0.2) | 31 (0.2) | 2 (0.2) | .960 |
| Symptoms | ||||
| Fever, n (%) | 10,176 (58.4) | 9,341 (57.1) | 835 (76.5) | <.0001 |
| Dry cough, n (%) | 12,125 (69.5) | 11,247 (68.8) | 878 (80.3) | <.0001 |
| Sore throat, n (%) | 5,331 (30.6) | 4,946 (30.3) | 385 (35.3) | .001 |
| Dyspnea, n (%) | 4,006 (23.0) | 3,175 (19.4) | 831 (76.0) | <.0001 |
| Diarrhea, n (%) | 2,454 (14.1) | 2,327 (14.2) | 127 (11.6) | .017 |
| Chest pain, n (%) | 2,958 (17.0) | 2,606 (15.9) | 352 (32.3) | <.0001 |
| Headache, n (%) | 13,125 (75.2) | 12,327 (75.4) | 798 (73.1) | .086 |
| Myalgia, n (%) | 8,020 (46.0) | 7,464 (45.7) | 556 (50.9) | .001 |
| Arthralgia, n (%) | 6,356 (36.5) | 5,826 (35.7) | 530 (48.5) | <.0001 |
| General malaise, n (%) | 5,673 (32.5) | 4,989 (30.5) | 684 (62.7) | <.0001 |
| Rhinorrhea, n (%) | 2,944 (16.9) | 2,776 (17.0) | 168 (15.4) | .175 |
| Polypnea, n (%) | 1,152 (6.6) | 850 (5.2) | 302 (27.7) | <.0001 |
| Vomiting, n (%) | 916 (5.3) | 844 (5.2) | 72 (6.6) | .040 |
| Abdominal pain, n (%) | 1,285 (7.4) | 1,197 (7.3) | 88 (8.1) | .364 |
| Conjunctivitis, n (%) | 871 (5.0) | 837 (5.1) | 34 (3.1) | .003 |
| Cyanosis, n (%) | 217 (1.2) | 160 (1.0) | 57 (5.2) | <.0001 |
| Anosmia, n (%) | 1,381 (9.1) | 1,337 (9.4) | 44 (4.6) | <.0001 |
SD: standard deviation; COPD: chronic obstructive pulmonary disease; HT: hypertension; HIV: human immunodeficiency virus.
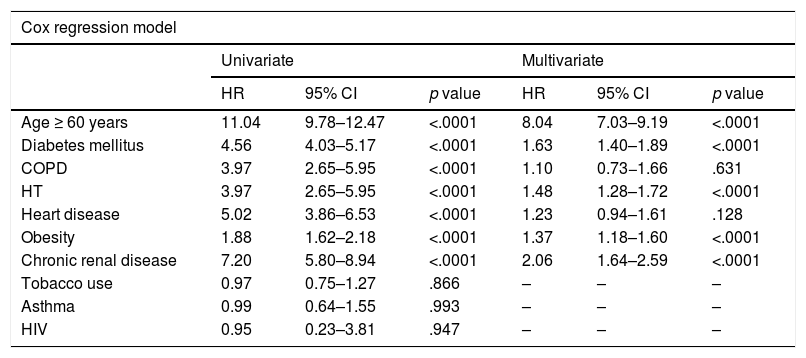
Of the data examined by means of the univariate Cox regression model, the following were associated with a statistically significant increase in risk of mortality (p < .0001): age over 60 years, diabetes mellitus, chronic obstructive pulmonary disease, systemic hypertension, heart disease, and chronic kidney disease. These variables were analyzed together by means of a multivariate Cox regression model. Age over 60 years had a hazard ratio (HR) of 8.04 with a 95% confidence interval (95% CI) of 7.03–9.19.
Among the comorbidities, the risk factors associated with mortality in patients with COVID-19 were: diabetes mellitus (HR = 1.63; 95% CI 1.40–1.89), systemic hypertension (HR = 1.48; 95% CI 1.28–1.72), obesity (HR = 1.37; 95% CI 1.18–1.60), and chronic kidney disease (HR = 2.06; 95% CI 1.64–2.59) (Table 2).
Risk factors associated with mortality in patients with COVID-19.
| Cox regression model | ||||||
|---|---|---|---|---|---|---|
| Univariate | Multivariate | |||||
| HR | 95% CI | p value | HR | 95% CI | p value | |
| Age ≥ 60 years | 11.04 | 9.78–12.47 | <.0001 | 8.04 | 7.03–9.19 | <.0001 |
| Diabetes mellitus | 4.56 | 4.03–5.17 | <.0001 | 1.63 | 1.40–1.89 | <.0001 |
| COPD | 3.97 | 2.65–5.95 | <.0001 | 1.10 | 0.73−1.66 | .631 |
| HT | 3.97 | 2.65–5.95 | <.0001 | 1.48 | 1.28–1.72 | <.0001 |
| Heart disease | 5.02 | 3.86–6.53 | <.0001 | 1.23 | 0.94–1.61 | .128 |
| Obesity | 1.88 | 1.62–2.18 | <.0001 | 1.37 | 1.18–1.60 | <.0001 |
| Chronic renal disease | 7.20 | 5.80–8.94 | <.0001 | 2.06 | 1.64–2.59 | <.0001 |
| Tobacco use | 0.97 | 0.75–1.27 | .866 | – | – | – |
| Asthma | 0.99 | 0.64–1.55 | .993 | – | – | – |
| HIV | 0.95 | 0.23–3.81 | .947 | – | – | – |
COPD: chronic obstructive pulmonary disease; HT: hypertension; HR: hazard ratio; 95% CI: 95% confidence interval; HIV: human immunodeficiency virus.
In regard to clinical characteristics, the most frequently reported symptoms in the literature worldwide were fever, cough, and fatigue, the same as in our study. Likewise, the most frequently associated comorbidities were hypertension, cardiovascular disease, and diabetes mellitus7. However, though these characteristics are similar among different countries and regions, mortality varies greatly8,9.
One probable explanation is that though comorbidities linked to SARS-CoV-2 infection increase mortality, age is a determining risk factor for a fatal outcome in patients with COVID-1910,11.
In a study in Brazil that included 2070 patients with this disease, though the proportion of diabetes (7.3%), obesity (0.2%), and kidney disease (1%) were lower than in our work, the mortality rate reported was 6%. Furthermore, 75% of patients who had a fatal outcome were in the group of patients over 60 years of age, many of whom had associated comorbidities12.
In a cohort of 13,842 patients in Mexico, 18% were in the group of patients older than 60 years. People with comorbidities had a greater risk of a fatal outcome, yet the reported mortality was 9.4% vs. 6.3% in our study. A likely explanation of the different in lethality could be the lower proportion of individuals over 60 years of age in our study (14%)13.
Along these lines, a transversal study which included 1,456 patients from different countries with a mortality rate of 26.4%, 80% of those who died were older than 65 years of age and the associated cardiovascular diseases and metabolic diseases increased mortality14.
When comparing our study to the work by Parra-Bracamonte et al.15, some interesting points can be seen. Though the mean age of the population studied was similar, the mortality rate was significantly different: 11.5% vs. 6.3% in our analysis.
This could be due to the lower proportion of people over 60 years of age with COVID-19 in our study (14% vs. 18.5%) as well as the lower percentage of individuals in our analysis with diabetes (10.9% vs. 16.2%), hypertension (13.5% vs. 20%), obesity (11.6% vs. 19.2%), and chronic kidney disease (1.4% vs. 2%).
These differences regarding the population with SARS-CoV-2 infection in our region compared to the rest of Mexico could be a result of the strategies implemented by the healthcare authorities to protect the at-risk population.
It can be observed that, regardless of the geographic region, the presence of comorbidities in patients with COVID-19 is a risk factor for mortality and an important associated factor which substantially increases this risk in people over 60 years of age.
ConclusionsIn conclusion, diabetes mellitus, systemic hypertension, obesity, and chronic kidney disease increase mortality in patients with COVID-19 among the population of Coahuila (Mexico). However, age over 60 years is the factor which most contributes to risk of death. It is important to continue applying strategies aimed at protecting this vulnerable population.
We recognize that our study has some limitations, such as its retrospective nature and the fact that the variables analyzed were obtained from an electronic database, which hindered patient follow-up. Therefore, more studies in different populations are needed in order to identify modifiable factors and implement strategies that impact patient survival.
FundingThe research has not received specific grants from agencies in the public, commercial, or non-profit sectors.
Conflicts of interestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Salinas-Aguirre JE, Sánchez-García C, Rodríguez-Sanchez R, Rodríguez-Muñoz L, Díaz-Castaño A, Bernal-Gómez R. Características clínicas y comorbilidades asociadas a mortalidad en pacientes con COVID-19 en Coahuila (México). Rev Clin Esp. 2022;222:288–292.