Systemic capillary leak syndrome (SCLS), also called Clarkson’s disease, is a severe, rare disease characterized by hypovolemic shock secondary to capillary leak which occurs in the context of monoclonal gammopathy1. It usually has a triggering factor, which tends to be an infection (generally viral). Its course is recurrent and it responds adequately to immunoglobulins (Ig) via intravenous route of administration (IV Ig)1. We conducted a scoping review and report the case of a patient who developed this disease in the context of a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection who, in the previous days, had received a COVID-19 vaccine.
The patient is a 38-year-old male who consulted with clinical symptoms that had been ongoing for five days characterized by intense pain in both lower limbs in addition to general malaise, arthromyalgia, diarrhea, and some isolated episodes of fever. He had received the second dose of the BNT162b2 (Pfizer-BioNTech) vaccine six days before the admission.
In the emergency room, hypotension (72/51 mmHg), pulse oximetry of 98%, sinus tachycardia (123 bpm), and poor peripheral perfusion were observed. He presented with a capillary refill greater than 5 s and coldness of the lower limbs. Bilateral femoral pulses were present and pedal pulses were not very perceptible. Both calves were hardened. Resuscitation was started with 2 L of crystalloid solution; despite this, the patient required vasopressors.
Of note on the blood test was hemoglobin of 23.6 g/dL (hematocrit 70%), hypoalbuminemia of 1.7 g/dL, hypoproteinemia of 3.76 g/dL, high lactic acid metabolic acidosis with serum lactate of 6.88 mmol/L, type III acute kidney injury (AKI), as per the Acute Kidney Injury Network (AKIN) classification, of a prerenal profile (urine sodium <3 mmol/L) without proteinuria or albuminuria, and homeostasis abnormalities (hyponatremia, hypokalemia, and hyperphosphatemia) with normal serum osmolarity.
A Doppler echocardiogram and CT angiogram ruled out vascular disease in the lower limbs. On the full body CT scan, a diffuse bilateral miliary pattern was observed that was compatible with SARS-CoV-2 pneumonia, which was confirmed with a positive polymerase chain reaction (PCR) test of nasopharyngeal exudate.
The patient was admitted to the intensive care unit (ICU) with a Simplified Acute Physiology Score (SAPS) II of 61 points and a Sequential Organ Failure Assessment (SOFA) score of 7 points. A serum protein electrophoresis test showed hypogammaglobulinemia of 9.4% (range 11.1–18.8) with an immunoelectrophoresis which detected clonality in IgA and IgG kappa and negative cryoglobulins. Other types of erythrocytosis such as polycythemia vera were ruled out as mutations of the V617F gene or exon 12 of the JAK2 gene were not detected; mutations in the BCR-ABL gene were also not found. The HIV, HBV, and HCV serology tests were negative.
At 48 h from admission, the patient developed hypoxemic respiratory failure which required starting invasive mechanical ventilation. The kidney failure improved following initial resuscitation, but the patient presented with another episode of deterioration secondary to rhabdomyolysis, with CK elevation up to 39,000 U/L that required continuous renal replacement therapy for 96 h.
Faced with the risk of compartment shock, compartment pressure was intermittently monitored in both calves, with values within normal range at all times. Lastly, the patient progressed favorable from the organ failure and was extubated as scheduled on the sixth day. He was discharged to the hospitalization ward on the ninth day of ICU admission.
The diagnosis of SCLS was made after ruling out other more common etiologies (sepsis, vascular disease, nephrotic syndrome, hyperviscosity syndromes). The patient presented with criteria compatible with hypovolemic shock, increased hematocrit, dehydration, and hypoalbuminemia in the context of hypogammaglobulinemia and clonality in IgG and IgA kappa1. Given that the most frequent trigger of these episodes is viral infections and that our patient had a positive SARS-CoV-2 PCR test, the infection was attributed as the cause of the SCLS. However, it must be noted that a case related to BNT162b2 vaccination was recently reported, although that case was in a patient with previous episodes of SCLS2.
Our patient required respiratory, hemodynamic, and renal support and developed rhabdomyolysis, but not compartment syndrome. There is evidence on the use of IV Ig for preventing episodes of severe SCLS, though its use in the acute phase is controversial and it is used as rescue therapy in most cases1. The use of Ig can be dangerous for patients with prerenal acute kidney injury with rhabdomyolysis1 and for this reason, it was not administered to our patient.
It is believed that the syndrome is due to an exaggerated response to inflammatory changes. This has been attributed to genetic defects within the endothelium that have been studied in rats and which predispose individuals to accelerated breakage of the vascular barrier, which makes the host more susceptible to developing SCLS3.
In one of the largest registries of SCLS analyzed by Pineton de Chambrun et al.1 in 2017, a mortality rate of 18.6% was found and compartment syndrome was the most frequent complication (20.3%). Kidney failure with a need for continuous renal replacement therapy is strongly associated with mortality.
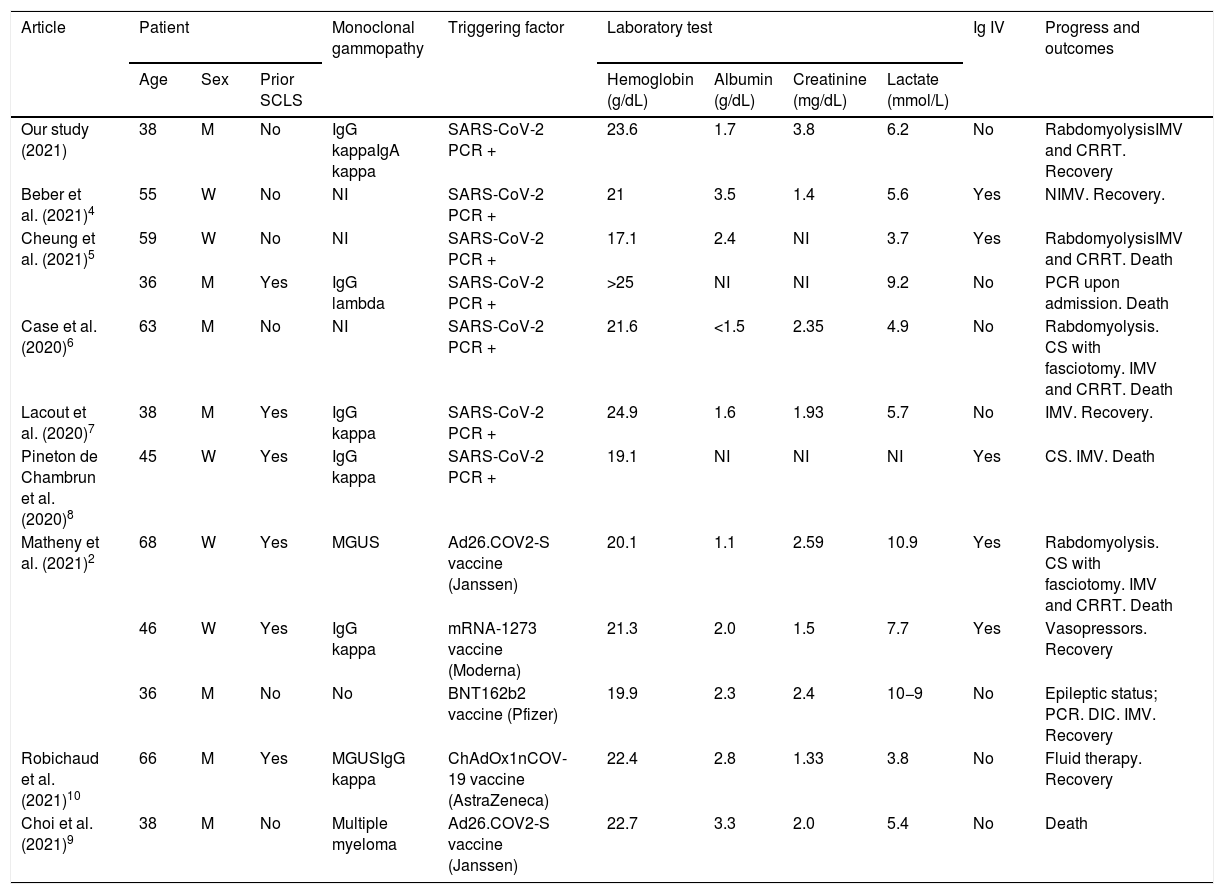
We conducted a review of the literature available to date (October 2021) on cases of SCLS related to SARS-CoV-2 infection or COVID-19 vaccination. The results are summarized in Table 1, where we list the patient characteristics as well as their progress and outcome. In total, with our case, seven patients with SCLS after SARS-CoV-2 infection4–8 and five patients with SCLS after SARS-CoV-2 vaccination have been described: two with Ad26.COV2-S (Janssen)2,9, one with ChAdOx1nCOV-19 (AstraZeneca)10, and two with mRNA vaccines (one Moderna and one Pfizer)2.
Characteristics of systemic capillary leak syndrome (SCLS) in cases (with SARS-CoV-2 infection or COVID-19 vaccination) described in the literature.
| Article | Patient | Monoclonal gammopathy | Triggering factor | Laboratory test | Ig IV | Progress and outcomes | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Sex | Prior SCLS | Hemoglobin (g/dL) | Albumin (g/dL) | Creatinine (mg/dL) | Lactate (mmol/L) | |||||
| Our study (2021) | 38 | M | No | IgG kappaIgA kappa | SARS-CoV-2 PCR + | 23.6 | 1.7 | 3.8 | 6.2 | No | RabdomyolysisIMV and CRRT. Recovery |
| Beber et al. (2021)4 | 55 | W | No | NI | SARS-CoV-2 PCR + | 21 | 3.5 | 1.4 | 5.6 | Yes | NIMV. Recovery. |
| Cheung et al. (2021)5 | 59 | W | No | NI | SARS-CoV-2 PCR + | 17.1 | 2.4 | NI | 3.7 | Yes | RabdomyolysisIMV and CRRT. Death |
| 36 | M | Yes | IgG lambda | SARS-CoV-2 PCR + | >25 | NI | NI | 9.2 | No | PCR upon admission. Death | |
| Case et al. (2020)6 | 63 | M | No | NI | SARS-CoV-2 PCR + | 21.6 | <1.5 | 2.35 | 4.9 | No | Rabdomyolysis. CS with fasciotomy. IMV and CRRT. Death |
| Lacout et al. (2020)7 | 38 | M | Yes | IgG kappa | SARS-CoV-2 PCR + | 24.9 | 1.6 | 1.93 | 5.7 | No | IMV. Recovery. |
| Pineton de Chambrun et al. (2020)8 | 45 | W | Yes | IgG kappa | SARS-CoV-2 PCR + | 19.1 | NI | NI | NI | Yes | CS. IMV. Death |
| Matheny et al. (2021)2 | 68 | W | Yes | MGUS | Ad26.COV2-S vaccine (Janssen) | 20.1 | 1.1 | 2.59 | 10.9 | Yes | Rabdomyolysis. CS with fasciotomy. IMV and CRRT. Death |
| 46 | W | Yes | IgG kappa | mRNA-1273 vaccine (Moderna) | 21.3 | 2.0 | 1.5 | 7.7 | Yes | Vasopressors. Recovery | |
| 36 | M | No | No | BNT162b2 vaccine (Pfizer) | 19.9 | 2.3 | 2.4 | 10−9 | No | Epileptic status; PCR. DIC. IMV. Recovery | |
| Robichaud et al. (2021)10 | 66 | M | Yes | MGUSIgG kappa | ChAdOx1nCOV-19 vaccine (AstraZeneca) | 22.4 | 2.8 | 1.33 | 3.8 | No | Fluid therapy. Recovery |
| Choi et al. (2021)9 | 38 | M | No | Multiple myeloma | Ad26.COV2-S vaccine (Janssen) | 22.7 | 3.3 | 2.0 | 5.4 | No | Death |
CA: cardiac arrest; CRRT: continuous renal replacement therapy; CS: compartment syndrome; DIC: disseminated intravascular coagulation; F: female; IMV: invasive mechanical ventilation; IV Ig: immunoglobulin via intravenous route of administration; M: male; MGUS: monoclonal gammopathy of undetermined significance; NI: not indicated; NIMV: non-invasive mechanical ventilation; SARS-CoV-2 PCR: severe acute respiratory syndrome coronavirus 2 polymerase chain reaction.
There is a mortality rate of 50% in the cases summarized in Table 1. Two of five patients who developed SCLS after vaccination and four of seven cases secondary to SARS-CoV-2 infection died.
Among the cases analyzed (Table 1), six patients had had episodes of SCLS previously, with another episode triggered after SARS-CoV-2 infection or vaccination. However, five patients did not have any previous episodes, with the diagnostic challenge this entails.
After a first episode of SCLS, follow-up should be provided to monitor recurrence and provide prophylaxis in cases in which it is needed. In patients with prior episodes of SCLS, the option of administering IV Ig as prophylaxis before administering COVID-19 vaccines should be evaluated.
SCLS is a rare disease but has severe clinical implications. Both SARS-CoV-2 infection and COVID-19 vaccination are possible triggering factors for this syndrome. Therefore, it is advisable to keep it in mind in the diagnostic and treatment approach.
We would like to thank the Intensive Medicine Department of the “Complejo Hospitalario Universitario de Toledo” for their help in the writing of this article.
Please cite this article as: Buj M, Morales-Varas G, Pedrosa-Guerrero A, Alonso-Ciria E. Síndrome de fuga capilar sistémica tras infección por SARS-CoV-2 y tras vacunación contra COVID-19: una revisión de alcance a propósito de un caso. Rev Clin Esp. 2022;222:374–376.