This article aims to assess the utility of CURB-65 in predicting 30-day mortality in adult patients hospitalized with COVID-19.
MethodsThis work is a cohort study conducted between March 1 and April 30, 2020 in Ecuador.
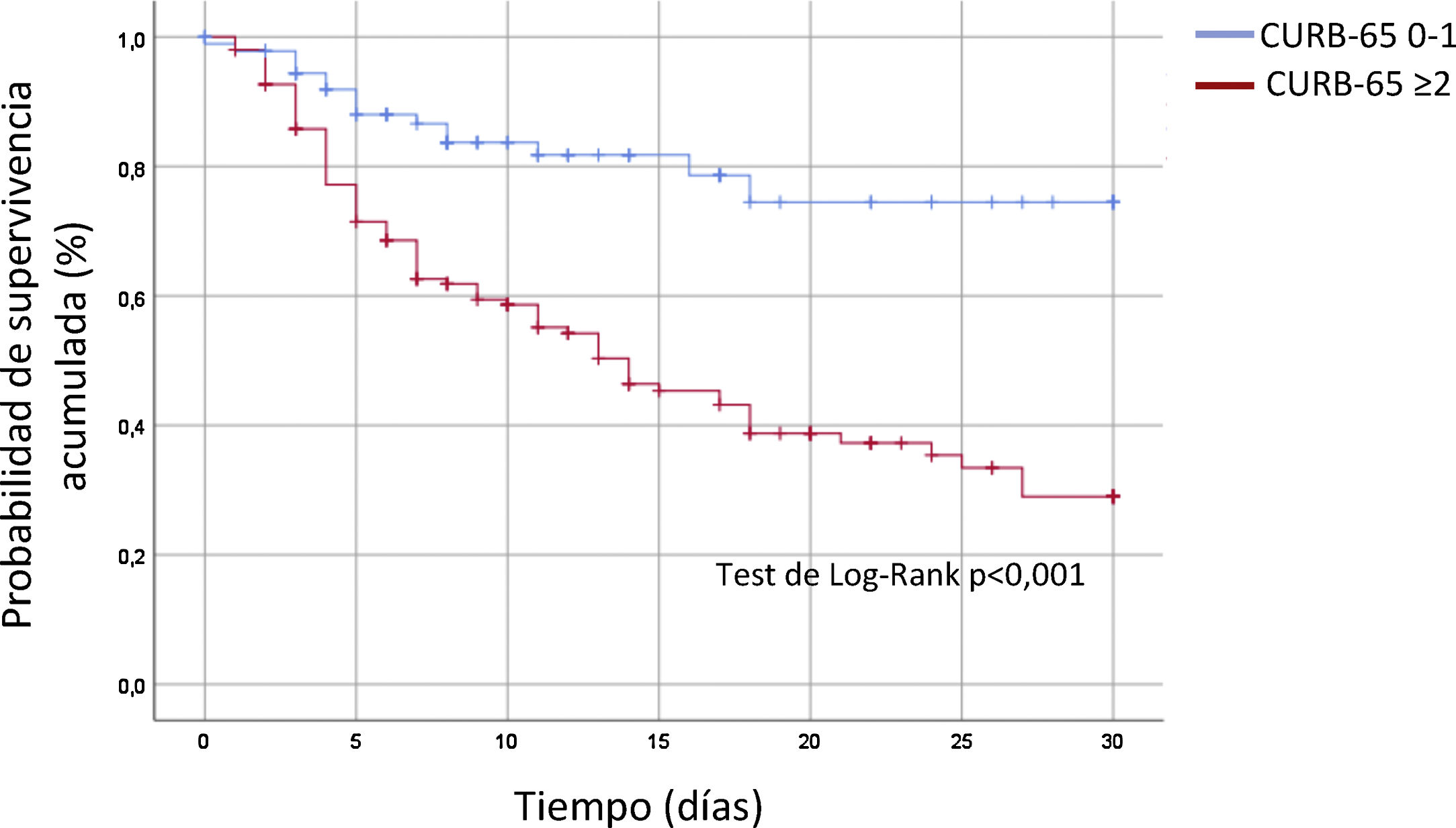
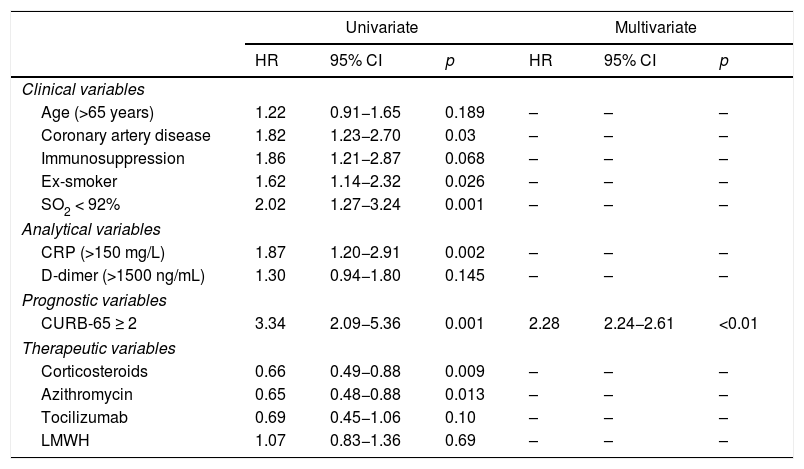
ResultsA total of 247 patients were included (mean age 60 ± 14 years, 70% men, overall mortality 41.3%). Patients with CURB-65 ≥ 2 had a higher mortality rate (57 vs. 17%, p < .001) that was associated with other markers of risk: advanced age, hypertension, overweight/obesity, kidney failure, hypoxemia, requirement for mechanical ventilation, or onset of respiratory distress.
ConclusionsCURB-65 ≥ 2 was associated with higher 30-day mortality on the univariate (Kaplan–Meier estimator) and multivariate (Cox regression) analysis.
Valorar la utilidad del CURB-65 para predecir la mortalidad a 30 días en pacientes adultos hospitalizados con COVID-19.
MétodosCohorte realizada entre el 1 de marzo y el 30 de abril de 2020 en Ecuador.
ResultadosSe incluyeron 247 pacientes (edad media 60 ± 14 años, 70% varones, mortalidad global 41,3%). Los pacientes con CURB-65 ≥ 2 presentaron mayor mortalidad (57 vs. 17%, p < 0,001), en asociación con otros marcadores de riesgo: edad avanzada, hipertensión arterial, sobrepeso/obesidad, fracaso renal, hipoxemia, requerimiento de ventilación mecánica o desarrollo de distrés respiratorio.
ConclusionesEn el análisis univariado (Kaplan–Meier) y multivariado (regresión de Cox) el CURB-65 ≥ 2 se relacionó con una mayor mortalidad a 30 días.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<